Maryland Chronic Wasting Disease Detected in 25 Deer
Chronic Wasting Disease (CWD) In Maryland
Deer Hunters and CWD
- Avoid shooting or handling a deer that appears sick.
- Wear latex or rubber gloves when field-dressing or butchering deer.
- Remove all internal organs.
- Remove the meat from the bones and spinal column if home processing a deer
- Do not use household knives or utensils when field-dressing or home processing a deer.
- Avoid cutting through bones or the spinal column (backbone).
- If you saw off antlers or through a bone, or if you sever the spinal column with a knife, be sure to disinfect these tools prior to using them for the butchering or removal of meat.
- Always wash hands and instruments thoroughly after dressing and processing game meat.
- Use a 50/50 solution of household chlorine bleach and water to disinfect tools and work surfaces. Wipe down counters and let them dry; soak knives for one hour.
Deer Urine Lures and CWD
- Whenever possible, avoid using natural urine lures and instead use synthetic lures. Research has shown synthetic lures to be as effective as natural lures.
- Hunters should avoid placing deer lures on the ground or on vegetation where deer can come into contact with them. Deer lures can be safely placed above deer height, yet still allow air currents to disperse the scent and attract deer.
- Hunters should not place urine-based lures on their skin or clothing.
CWD Management
Whole deer carcasses or deer parts cannot be transported out of the CWDMA, except for:
- Meat with no part of the spinal column, backbone, or head attached,
- Hind quarters and front shoulders with no spinal column or backbone attached, (hunters MUST have checked in their deer and obtained a confirmation number in order to transport a quartered deer)
- Cleaned hide with no head attached,
- Skull plate cleaned of all meat and brain tissue,
- Antlers with no meat or soft tissue attached,
- Finished taxidermy mounts or tanned hides,
- Whole deer carcasses or parts being transported directly to the meat processors or taxidermists listed below, or to the landfill located within Allegany or Washington County.
- Currently, the following taxidermists and meat processors are approved to prepare or process deer carcasses or deer parts taken from within Maryland’s CWDMA. This provision provides an opportunity for hunters harvesting deer within Maryland’s CWDMA to transport carcasses or other deer parts directly to one of these approved businesses for meat processing, taxidermy services or for preparation for transport to another taxidermist.
Meats Processors
B&B Country Meats, Frostburg, MD, 301-689-6225B&B Butchering, Orleans, MD, 301-478-2558Ernst Market, Clear Spring, MD, 301-842-2292Holsinger's Meats and Deli, Maugansville, MD 301-733-9262Sunnyland/Ray Burger's Meats, Williamsport, MD, 301-223-9637Wolfe's Deer Shop, Thurmont, MD, 240-549-2613
Taxidermists
Allegany County – Donnie Burley, Cumberland, MD, 301-707-6272Allegany County – Steven Fairgrieve, Barton, MD, 301-707-9261Allegany County – Robert Friend, Westernport, MD, 301-359-9784Allegany County – Richard Kroll, Barton, MD 301-359-5010Allegany County – Brian McKinley, Cumberland, MD, 240-580-4148Frederick County - Kline's Taxidermy, Smithsburg, MD, 301-416-0201Frederick County - Geisinger Taxidermy, Thurmont, MD, 301-271-0501Frederick County – Whitetail Studios, Thurmont, MD, 301-271-4858Washington County - Fairview Wildlife Studio, Hagerstown, MD, 301-791-1568Washington County - Millstone Taxidermy, Hancock, MD, 240-520-7226
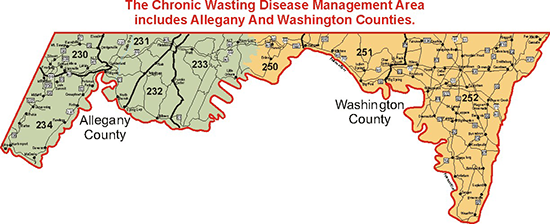
2019 Chronic Wasting Disease Management Area Map
Carcass Importation Ban
Taking Deer Carcasses out of Maryland
How You Can Help
Our ongoing studies will show whether the transmission of CWD into macaques and passage in transgenic mice represents a form of non-adaptive prion amplification, and whether macaque-adapted prions have the potential to infect mice expressing human PrP.
states.
***Subsequent testing resulted in the detection of pathologic lesion in unusual brain location and PrPsc detection by PMCA only.
*** IBNC Tauopathy or TSE Prion disease, it appears, no one is sure ***
http://www.plosone.org/annotation/listThread.action?root=86610
Diagnosis and Reporting of Creutzfeldt-Jakob DiseaseSingeltary, Sr et al. JAMA.2001; 285: 733-734. Vol. 285 No. 6, February 14, 2001 JAMA Diagnosis and Reporting of Creutzfeldt-Jakob DiseaseTo the Editor:In their Research Letter, Dr Gibbons and colleagues1 reported that the annual US death rate due to Creutzfeldt-Jakob disease (CJD) has been stable since 1985. These estimates, however, are based only on reported cases, and do not include misdiagnosed or preclinical cases. It seems to me that misdiagnosis alone would drastically change these figures. An unknown number of persons with a diagnosis of Alzheimer disease in fact may have CJD, although only a small number of these patients receive the postmortem examination necessary to make this diagnosis. Furthermore, only a few states have made CJD reportable. Human and animal transmissible spongiform encephalopathies should be reportable nationwide and internationally..Terry S. Singeltary, Sr Bacliff, Tex1. Gibbons RV, Holman RC, Belay ED, Schonberger LB. Creutzfeldt-Jakob disease in the United States: 1979-1998. JAMA. 2000;284:2322-2323.doi:10.1016/S1473-3099(03)00715-1 Copyright © 2003 Published by Elsevier Ltd. Newsdesk
Tracking spongiform encephalopathies in North AmericaXavier BoschAvailable online 29 July 2003.Volume 3, Issue 8, August 2003, Page 463“My name is Terry S Singeltary Sr, and I live in Bacliff, Texas. I lost my mom to hvCJD (Heidenhain variant CJD) and have been searching for answers ever since. What I have found is that we have not been told the truth. CWD in deer and elk is a small portion of a much bigger problem..” ............................January 28, 2003; 60 (2) VIEWS & REVIEWSMonitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United StatesErmias D. Belay, Ryan A. Maddox, Pierluigi Gambetti, Lawrence B. SchonbergerFirst published January 28, 2003, DOI: https://doi.org/10.1212/01.WNL.0000036913.87823.D6AbstractTransmissible spongiform encephalopathies (TSEs) attracted increased attention in the mid-1980s because of the emergence among UK cattle of bovine spongiform encephalopathy (BSE), which has been shown to be transmitted to humans, causing a variant form of Creutzfeldt-Jakob disease (vCJD). The BSE outbreak has been reported in 19 European countries, Israel, and Japan, and human cases have so far been identified in four European countries, and more recently in a Canadian resident and a US resident who each lived in Britain during the BSE outbreak. To monitor the occurrence of emerging forms of CJD, such as vCJD, in the United States, the Centers for Disease Control and Prevention has been conducting surveillance for human TSEs through several mechanisms, including the establishment of the National Prion Disease Pathology Surveillance Center. Physicians are encouraged to maintain a high index of suspicion for vCJD and use the free services of the pathology center to assess the neuropathology of clinically diagnosed and suspected cases of CJD or other TSEs.Received May 7, 2002. Accepted August 28, 2002.RE-Monitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United StatesTerry S. Singeltary, retired (medically)Published March 26, 200326 March 2003Terry S. Singeltary, retired (medically) CJD WATCHI lost my mother to hvCJD (Heidenhain Variant CJD). I would like to comment on the CDC's attempts to monitor the occurrence of emerging forms of CJD. Asante, Collinge et al [1] have reported that BSE transmission to the 129-methionine genotype can lead to an alternate phenotype that is indistinguishable from type 2 PrPSc, the commonest sporadic CJD. However, CJD and all human TSEs are not reportable nationally. CJD and all human TSEs must be made reportable in every state and internationally. I hope that the CDC does not continue to expect us to still believe that the 85%+ of all CJD cases which are sporadic are all spontaneous, without route/source. We have many TSEs in the USA in both animal and man. CWD in deer/elk is spreading rapidly and CWD does transmit to mink, ferret, cattle, and squirrel monkey by intracerebral inoculation. With the known incubation periods in other TSEs, oral transmission studies of CWD may take much longer. Every victim/family of CJD/TSEs should be asked about route and source of this agent. To prolong this will only spread the agent and needlessly expose others. In light of the findings of Asante and Collinge et al, there should be drastic measures to safeguard the medical and surgical arena from sporadic CJDs and all human TSEs. I only ponder how many sporadic CJDs in the USA are type 2 PrPSc?Reply to Singletary Ryan A. Maddox, MPH Other Contributors: Published March 26, 2003Mr. Singletary raises several issues related to current Creutzfeldt- Jakob disease (CJD) surveillance activities. Although CJD is not a notifiable disease in most states, its unique characteristics, particularly its invariably fatal outcome within usually a year of onset, make routine mortality surveillance a useful surrogate for ongoing CJD surveillance.[1] In addition, because CJD is least accurately diagnosed early in the course of illness, notifiable-disease surveillance could be less accurate than, if not duplicative of, current mortality surveillance.[1] However, in states where making CJD officially notifiable would meaningfully facilitate the collection of data to monitor for variant CJD (vCJD) or other emerging prion diseases, CDC encourages the designation of CJD as a notifiable disease.[1] Moreover, CDC encourages physicians to report any diagnosed or suspected CJD cases that may be of special public health importance (e.g...., vCJD, iatrogenic CJD, unusual CJD clusters).As noted in our article, strong evidence is lacking for a causal link between chronic wasting disease (CWD) of deer and elk and human disease,[2] but only limited data seeking such evidence exist. Overall, the previously published case-control studies that have evaluated environmental sources of infection for sporadic CJD have not consistently identified strong evidence for a common risk factor.[3] However, the power of a case-control study to detect a rare cause of CJD is limited, particularly given the relatively small number of subjects generally involved and its long incubation period, which may last for decades. Because only a very small proportion of the US population has been exposed to CWD, a targeted surveillance and investigation of unusual cases or case clusters of prion diseases among persons at increased risk of exposure to CWD is a more efficient approach to detecting the possible transmission of CWD to humans. In collaboration with appropriate local and state health departments and the National Prion Disease Pathology Surveillance Center, CDC is facilitating or conducting such surveillance and case- investigations, including related laboratory studies to characterize CJD and CWD prions.Mr. Singletary also expresses concern over a recent publication by Asante and colleagues indicating the possibility that some sporadic CJD cases may be attributable to bovine spongiform encephalopathy (BSE).[4] The authors reported that transgenic mice expressing human prion protein homozygous for methionine at codon 129, when inoculated with BSE prions, developed a molecular phenotype consistent with a subtype of sporadic CJD. Although the authors implied that BSE might cause a sporadic CJD-like illness among persons homozygous for methionine, the results of their research with mice do not necessarily directly apply to the transmission of BSE to humans. If BSE causes a sporadic CJD-like illness in humans, an increase in sporadic CJD cases would be expected to first occur in the United Kingdom, where the vast majority of vCJD cases have been reported. In the United Kingdom during 1997 through 2002, however, the overall average annual mortality rate for sporadic CJD was not elevated; it was about 1 case per million population per year. In addition, during this most recent 6-year period following the first published description of vCJD in 1996, there was no increasing trend in the reported annual number of UK sporadic CJD deaths.[3, 5] Furthermore, surveillance in the UK has shown no increase in the proportion of sporadic CJD cases that are homozygous for methionine (Will RG, National CJD Surveillance Unit, United Kingdom, 2003; personal communication)..References1. Gibbons RV, Holman RC, Belay ED, Schonberger LB. Diagnosis and reporting of Creutzfeldt-Jakob disease. JAMA 2001;285:733-734.2. Belay ED, Maddox RA, Gambetti P, Schonberger LB. Monitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United States. Neurology 2003;60:176-181.3. Belay ED. Transmissible spongiform encephalopathies in humans. Annu Rev Microbiol 1999;53:283-314.4. Asante EA, Linehan JM, Desbruslais M, et al. BSE prions propagate as either variant CJD-like or sporadic CJD-like prion strains in transgenic mice expressing human prion protein. EMBO J 2002;21:6358-6366.5. The UK Creutzfeldt-Jakob Disease Surveillance Unit. CJD statistics. Available at: http://www.cjd.ed.ac.uk/figures.htm. Accessed February 18, 2003.Competing Interests: None declared.Volume 2: Science4. The link between BSE and vCJDSummary 4.29 The evidence discussed above that vCJD is caused by BSE seems overwhelming. Uncertainties exist about the cause of CJD in farmers, their wives and in several abattoir workers. It seems that farmers at least might be at higher risk than others in the general population. 1 Increased ascertainment (ie, increased identification of cases as a result of greater awareness of the condition) seems unlikely, as other groups exposed to risk, such as butchers and veterinarians, do not appear to have been affected. The CJD in farmers seems to be similar to other sporadic CJD in age of onset, in respect to glycosylation patterns, and in strain-typing in experimental mice. Some farmers are heterozygous for the methionine/valine variant at codon 129, and their lymphoreticular system (LRS) does not contain the high levels of PrPSc found in vCJD.***>It remains a remote possibility that when older people contract CJD from BSE the resulting phenotype is like sporadic CJD and is distinct from the vCJD phenotype in younger people...endBSE INQUIRYSATURDAY, JUNE 23, 2018CDC***> Diagnosis of Methionine/Valine Variant Creutzfeldt-Jakob Disease by Protein Misfolding Cyclic AmplificationVolume 24, Number 7—July 2018 Dispatch
Diagnosis and Reporting of Creutzfeldt-Jakob Disease
 Maryland Deer Hunters' Attitudes Toward Chronic Wasting Disease
Maryland Deer Hunters' Attitudes Toward Chronic Wasting Disease
0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home