From: Terry Singeltary
To: michelle.carstensen
Cc: michael.crusan
Sent: Fri, Oct 11, 2019 1:07 pm
Subject: Minnesota Officials Burn, Bury, Worry As Chronic Wasting Spreads
Greetings Minnesota Officials Combating the cwd tse prion.
i 'liked' the dipsty dumpster proposal, as i cringed at that thought, but it was better than sitting idly by and doing nothing, more decades go by.
i cringed at the thought of open pyres burning cwd tse prion carcasses, even after the bse pyres warning, but here we are.
we have scientist and medical officials working in hazmat suits, and we have the common hunter and officials there from doing just the opposite.
confusing is an underestimation imo.
reminds me of the early days of the BSE epidemic.
Incinerators worked night and day burning cattle. Pictures of bovine funeral pyres led the news day after day as hundreds of herds were burnt. Farmers were ruined. Many have never recovered.
i have followed the mad cow tse prion follies since inception, and losing my mother to the hvCJD confirmed.
i have followed the science daily since that fateful day December 14, 1997.
science is a wonderful thing, if it's sound science, and not junk science, science bought and paid for by the industry.
what our fine federal friends have passed off as sound science about mad cow disease, was a joke, a sad and serious joke, that continues to help spread the tse prion.
some things you all may want to ponder, if you have not already...GOOD LUCK!...kindest regards, terry
Minnesota Officials Burn, Bury, Worry As Chronic Wasting Spreads
Oct 08, 2019 07:35PM ● By Editor

Marv Stroschein manages the Crow Wing County landfill. He lobbied for an extra careful approach for disposing of chronic wasting disease-positive deer carcasses. Photo: John Enger | MPR News
They’re discovering there is no perfect, affordable way to dispose of deer carcasses potentially infected with chronic wasting disease.‘Cover it up and we’re good’
By John Enger of Minnesota Public Radio News - October 8, 2019
Marv Stroschein and his Crow Wing County, Minn., landfill crew poured gallons of kerosene onto a huge pile of cordwood in an incinerator the size of a shipping container, then tossed in a road flare to light it up.
Supercharged with oxygen, temperatures inside the massive open-air incinerator top out at 2,300 degrees Fahrenheit. Stroschein needed at least 1,000 degrees — near the melting point of aluminum — to kill what he was hunting this day: prions, the deformed brain and nerve cells of deer carcasses infected with chronic wasting disease.
Since chronic wasting was discovered in the county earlier this year in a wild deer — the first wild deer case confirmed outside of southeastern Minnesota — Crow Wing officials have struggled for answers to the mess they believe is coming: disposing of thousands of infected or potentially infected deer carcasses.
Burning carcasses is inefficient, time-consuming and incredibly unsustainable. But after months of negotiation between the state Department of Natural Resources, county landfill officials and the Minnesota Pollution Control Agency, it’s the best anyone could do.
The central-Minnesota county offers a look at the nightmare challenges some Minnesota communities may soon face as they struggle to keep the disease in check and control the environmental contamination.
First found in wild herds in southeastern Minnesota in 2016, chronic wasting is a death sentence for the animals who contract it. There's no cure for the brain disease and no vaccine. The life expectancy of a CWD-positive deer is about two years.
At a minimum, there’s a fear it could destroy Minnesota’s $1 billion annual deer-hunting industry. While there’s currently no known crossover of the disease to humans, experts worry it could eventually jump species and find its way to humans.
So, the need for a scientifically sound way to dispose of carcasses is critical.
Burning deer bones is relatively new in Minnesota. Most hunters just toss carcasses out in the woods when they’re done processing the meat.
But tossing out deer bones is risky where chronic wasting disease is present.
Prions are extraordinarily stubborn in their survival. They can linger for years in the soil long after their hosts are dead, contaminating other deer and the environment around them.
In the last legislative session, Minnesota lawmakers created a deer dumpster program to remedy this problem.
They set aside $50,000 to place special plastic-lined dumpsters in chronic-wasting-infected areas, lifting the idea from Wisconsin landowner Doug Duren, who theorized that if hunters threw their carcasses into dumpsters, they wouldn’t throw them out onto the landscape and the disease might not spread so fast.
It’s turned out not to be so simple.

A small load of deer parts arrives at the Crow Wing County landfill late last month. Tim Stroschein directs the truck to the incinerator. Photo: John Enger | MPR News
“This whole thing is complicated,” said Minnesota DNR wildlife health group leader Michelle Carstensen. “I never thought I’d know so much about dumpsters and landfills.”
Carstensen was put in charge of emptying the deer dumpsters.
It was easy to do in southeastern Minnesota, where chronic wasting disease has existed for years. There was already a massive industrial incinerator to deal with animals taken in federal culling efforts.
But the infection in Crow Wing County is much more recent. A doe tested positive in Crow Wing earlier this year. Now, every deer shot within a 13-mile radius of the infection has to be tested.
By law, hunters have to either leave the carcasses exactly where the animal was shot, or bring them to a deer dumpster.
“When it comes to burying weird things, landfills and the Pollution Control Agency already have a process,” Carstensen said. “I though they were just going to bury the deer on a dedicated spot on the landfill, put clay-lined materials down and cover it up and we’re good.”
But Stroschein turned her down. And thus began a monthslong negotiation.
Hard to kill
Stroschein — a careful man who’s been in the landfill business for 37 years — told Carstensen he couldn’t live with himself if he took an infected deer and then allowed prions to escape into the environment.
It’s an understandable position. Prions are famously hard to neutralize. They can pass unharmed through the digestive system of a predator, withstand up to 1,000 degree temperatures and exist on the land for many years.
Carstensen showed him scientific studies proving that it’s safe to bury infected deer in conventional landfills. He showed her the 40-acre field where he sprays wastewater from his trash pits.
He said he worried prions would get onto the grass and then back into wild deer.
Carstensen suggested he just fence in the irrigation zone. He built the fence, but still worried it wasn’t good enough. The negotiations spawned a work group of stakeholders. They had meetings. They brought in medical and prion experts.
Carstensen looked into trucking the dumpsters to a landfill in the next county over, but officials there were nervous, too. They wondered if Crow Wing knew something they didn’t.
“I thought, ‘Oh no! We’re screwed!’” Carstensen said. “We’re going to be like Wisconsin.”
Even after decades of fighting the disease, Wisconsin’s system for disposing of infected animals is woefully inadequate. Duren’s deer dumpster program is still tiny, and once the dumpsters are full there are very few places to empty them. In all of Wisconsin, just 13 landfills accept deer waste.
Wisconsin DNR solid waste coordinator Dan Kroll said it didn’t used to be that way. But recently, a few private landfills announced they were no longer accepting carcasses. They were afraid of being held liable for escaped prions. After that, dozens of others got spooked.
“We just had our two biggest landfill operators back out,” he said. “They don’t take deer anymore.”
In some parts of the state, hunters now have to drive 80 miles to get rid of their bones. Kroll said they don’t do it. They either throw their carcasses in rural ditches or smuggle them into prohibited landfills disguised as household trash.
Carstensen didn’t want the same thing to happen in Minnesota.
If a single landfill turned down deer carcasses, she worried the rest would fall like dominoes. Finally, weeks before the opening of archery season, she offered to give the Crow Wing landfill a 15-year-old, disused DNR incinerator, and the landfill took it.
“It’s overkill,” she said, “But landfill operators talk to each other.”
‘Huge issue’
The best way to get rid of CWD-positive material, is with an alkaline hydrolysis digester. The veterinary wing of the University of Minnesota has one in St. Paul to dispose of infectious animal carcasses.
It’s basically a giant pressure cooker full of lye. Infected meat and bone go in. Inert slush comes out. But digesters are incredibly expensive. It’s not a solution that could be scaled up to handle thousands of deer.
For Crow Wing County, the safest, most practical solution was to build a giant, controlled inferno.
Still, the incinerator itself has been plagued with technical issues. The first burn was a disaster, Stroschein recalled.
“There was all this water in the dumpster,” he said. “Mixed in with the deer, it basically put out the fire. The blower barely got it going again.”
The second round went a bit better.
In late September, however, he and the landfill crew loaded up the incinerator with wood for their third deer burning attempt and the fire didn’t want to start.
The flare they’d tossed in went out before the cordwood ignited. Stroschein’s son Tim had to climb up on the machine with a propane torch to get it going. A little later the blower stopped working. The diesel engine was out of fuel, or maybe just broken. No one was sure.

When the kerosene and road flares don’t work, Tim Stroschein uses a blow torch to light the fire. Photo: John Enger | MPR News
When they did get it running, the bone delivery truck slated to bring 12-cubic yards of possibly infected deer spines and heads from a processing facility in Emily, Minn., was nowhere to be found.
Stroschein made calls and paced around as the fire burned.
The truck arrived four hours late with just two small deer-rib cages to feed into the giant fire.
Stroschein said the system will get more efficient over time. It’ll have to.
Chronic wasting disease is still spreading. In the years to come, more deer carcasses will likely be heading to more landfills, and four cords of firewood per deer is not a scalable ratio.
“When it comes to landfills and carcass disposal, scalability is a huge issue that needs to be addressed,” said Michael Osterholm, director of the University of Minnesota Center for Infectious Disease Research and Policy. “How do we — in a CWD positive area — best dispose of these carcasses? There’s a lot more work that needs to be done.”
Osterholm is among the experts who worry that chronic wasting will find its way to humans the way “mad cow disease” in the United Kingdom became variant Creutzfeldt-Jakob disease.
“There are a lot of challenges in attempting to deal with carcasses of CWD-infected deer,” Osterholm added, “but I’m confident that Crow Wing County is doing as well as anyone could.”
Strochein said he’ll burn roughly 5,000 deers-worth of bones and heads this hunting season alone at the Crow Wing landfill. He’s determined that chronic wasting will not spread on his watch.
“Nothing’s getting sick from these carcasses when we’re done with them,” he said.
To read the original article and hear an audio report of this story follow this link to the MPR News website.
Subject: Aerosol transmission tse prion
In summary, our results establish aerosols as a surprisingly efficient modality of prion transmission. This novel pathway of prion transmission is not only conceptually relevant for the field of prion research, but also highlights a hitherto unappreciated risk factor for laboratory personnel and personnel of the meat processing industry. In the light of these findings, it may be appropriate to revise current prion-related biosafety guidelines and health standards in diagnostic and scientific laboratories being potentially confronted with prion infected materials. While we did not investigate whether production of prion aerosols in nature suffices to cause horizontal prion transmission, the finding of prions in biological fluids such as saliva, urine and blood suggests that it may be worth testing this possibility in future studies.
Professor Aguzzi commented;
“We even showed that a prion AEROSOL will infect 100% of mice within 10 seconds of exposure” end...tss
FRIDAY, OCTOBER 04, 2019
Inactivation of chronic wasting disease prions using sodium hypochlorite
i think some hunters that don't read this carefully are going to think this is a cure all for cwd tse contamination. IT'S NOT!
first off, it would take a strong bleach type sodium hypochlorite, that is NOT your moms bleach she uses in her clothes, and store bought stuff.
Concentrated bleach is an 8.25 percent solution of sodium hypochlorite, up from the “regular bleach” concentration of 5.25 percent.Nov 1, 2013 https://waterandhealth.org/disinfect/high-strength-bleach-2/
second off, the study states plainly;
''We found that a five-minute treatment with a 40% dilution of household bleach was effective at inactivating CWD seeding activity from stainless-steel wires and CWD-infected brain homogenates. However, bleach was not able to inactivate CWD seeding activity from solid tissues in our studies.''
''We initially tested brains from two CWD-infected mice and one uninfected mouse using 40% bleach for 5 minutes. The results from these experiments showed almost no elimination of prion seeding activity (Table 4). We then increased the treatment time to 30 minutes and tested 40% and 100% bleach treatments. Again, the results were disappointing and showed less than a 10-fold decrease in CWD-seeding activity (Table 4). Clearly, bleach is not able to inactivate prions effectively from small brain pieces under the conditions tested here.''
''We found that both the concentration of bleach and the time of treatment are critical for inactivation of CWD prions. A 40% bleach treatment for 5 minutes successfully eliminated detectable prion seeding activity from both CWD-positive brain homogenate and stainless-steel wires bound with CWD. However, even small solid pieces of CWD-infected brain were not successfully decontaminated with the use of bleach.''
i think with all the fear from recent studies, and there are many, of potential, or likelihood of zoonosis, if it has not already happened as scjd, i think this study came out to help out on some of that fear, that maybe something will help, but the study plainly states it's for sure not a cure all for exposure and contamination of the cwd tse prion on surface materials. imo...terry
first off, it would take a strong bleach type sodium hypochlorite, that is NOT your moms bleach she uses in her clothes, and store bought stuff.
Concentrated bleach is an 8.25 percent solution of sodium hypochlorite, up from the “regular bleach” concentration of 5.25 percent.Nov 1, 2013 https://waterandhealth.org/disinfect/high-strength-bleach-2/
second off, the study states plainly;
''We found that a five-minute treatment with a 40% dilution of household bleach was effective at inactivating CWD seeding activity from stainless-steel wires and CWD-infected brain homogenates. However, bleach was not able to inactivate CWD seeding activity from solid tissues in our studies.''
''We initially tested brains from two CWD-infected mice and one uninfected mouse using 40% bleach for 5 minutes. The results from these experiments showed almost no elimination of prion seeding activity (Table 4). We then increased the treatment time to 30 minutes and tested 40% and 100% bleach treatments. Again, the results were disappointing and showed less than a 10-fold decrease in CWD-seeding activity (Table 4). Clearly, bleach is not able to inactivate prions effectively from small brain pieces under the conditions tested here.''
''We found that both the concentration of bleach and the time of treatment are critical for inactivation of CWD prions. A 40% bleach treatment for 5 minutes successfully eliminated detectable prion seeding activity from both CWD-positive brain homogenate and stainless-steel wires bound with CWD. However, even small solid pieces of CWD-infected brain were not successfully decontaminated with the use of bleach.''
i think with all the fear from recent studies, and there are many, of potential, or likelihood of zoonosis, if it has not already happened as scjd, i think this study came out to help out on some of that fear, that maybe something will help, but the study plainly states it's for sure not a cure all for exposure and contamination of the cwd tse prion on surface materials. imo...terry
FRIDAY, OCTOBER 04, 2019
Inactivation of chronic wasting disease prions using sodium hypochlorite
Subject: BSE Inquiry Incineration TSE Prion Survival
BSE Inquiry Incineration
understand two things, these are old documents, some science has changed, especially with cwd tse prion...terry
BSE INQUIRY 1989 TO ...2013
The BSE Inquiry / Statement No 19B (supplementary) Dr Alan Colchester Issued 06/08/1999 (not scheduled to give oral evidence)
SECOND STATEMENT TO THE BSE INQUIRY
Dr A Colchester BA BM BCh PhD FRCP Reader in Neurosciences & Computing, University of Kent at Canterbury; Consultant Neurologist, Guy’s Hospital London and William Harvey Hospital Ashford April 1999
snip...
88. Natural decay: Infectivity persists for a long time in the environment. A study by Palsson in 1979 showed how scrapie was contracted by healthy sheep, after they had grazed on land which had previously been grazed by scrapie-infected sheep, even though the land had lain fallow for three years before the healthy sheep were introduced. Brown also quoted an early experiment of his own (1991), where he had buried scrapie-infected hamster brain and found that he could still detect substantial infectivity three years later near where the material had been placed. 89. Potential environmental routes of infection: Brown discusses the various possible scenarios, including surface or subsurface deposits of TSE-contaminated material, which would lead to a build-up of long-lasting infectivity. Birds feeding on animal remains (such as gulls visiting landfill sites) could disperse infectivity. Other animals could become vectors if they later grazed on contaminated land. "A further question concerns the risk of contamination of the surrounding water table or even surface water channels, by effluents and discarded solid wastes from treatment plants. A reasonable conclusion is that there is a potential for human infection to result from environmental contamination by BSE-infected tissue residues. The potential cannot be quantified because of the huge numbers of uncertainties and assumptions that attend each stage of the disposal process". These comments, from a long established authority on TSEs, closely echo my own statements which were based on a recent examination of all the evidence. 90. Susceptibility: It is likely that transmissibility of the disease to humans in vivo is probably low, because sheep that die from scrapie and cattle that die from BSE are probably a small fraction of the exposed population. However, no definitive data are available.
91. Recommendations for disposal procedures: Brown recommends that material which is actually or potentially contaminated by BSE should be: 1) exposed to caustic soda; 2) thoroughly incinerated under carefully inspected conditions; and 3) that any residue should be buried in landfill, to a depth which would minimise any subsequent animal or human exposure, in areas that would not intersect with any potable water-table source.
92. This review and recommendations from Brown have particular importance. Brown is one of the world's foremost authorities on TSEs and is a senior researcher in the US National Institutes of Health (NIH). It is notable that such a respected authority is forthright in acknowledging the existence of potential risks, and in identifying the appropriate measures necessary to safeguard public health. Paper by SM Cousens, L Linsell, PG Smith, Dr M Chandrakumar, JW Wilesmith, RSG Knight, M Zeidler, G Stewart, RG Will, "Geographical distribution of variant CJD in the UK (excluding Northern Ireland)". Lancet 353:18-21, 2 nd January 1999 93. The above paper {Appendix 41 (02/01/99)} (J/L/353/18) examined the possibility that patients with vCJD (variant CJD) might live closer to rendering factories than would be expected by chance. All 26 cases of vCJD in the UK with onset up to 31 st August 1998 were studied. The incubation period of vCJD is not known but by analogy with other human TSEs could lie within the range 5-25 years. If vCJD had arisen by exposure to rendering products, such exposure might plausibly have occurred 8-10 years before the onset of symptoms. The authors were able to obtain the addresses of all rendering plants in the UK which were in production in 1988. For each case of vCJD, the distance from the place of residence on 1st January 1998 to the nearest rendering plant was calculated
snip...
BSE INQUIRY DATA 1989 through the 1990’s REPORT ON BOVINE CARCASE INCINERATION, incinerations temps., plume, etc. ...tss
some unofficial info. from a source on the inside looking out;
Confidential!!!!
As early as 1992-3 there had been long studies conducted on small pastures containing scrapie infected sheep at the sheep research station associated with the Neuropathogenesis Unit in Edinburgh, Scotland. Whether these are documented...I don't know. But personal recounts both heard and recorded in a daily journal indicate that leaving the pastures free and replacing the topsoil completely at least 2 feet of thickness each year for SEVEN years....and then when very clean (proven scrapie free) sheep were placed on these small pastures.... the new sheep also broke with scrapie and passed it to offspring. I am not sure that TSE contaminated ground could ever be free of the agent!! A very frightening revelation!!!
xxxxxxxxxxxend...tss...personal communication...tss
more here;
INCINERATION TEMPS
requirements include;
a. after burning to the range of 800 to 1000*C to eliminate smell;
well heck, this is just typical public relations fear factor control. do you actually think they would spend the extra costs for fuel, for such extreme heat, just to eliminate smell, when they spread manure all over your veg's. i think not. what they really meant were any _TSE agents_.
b. Gas scrubbing to eliminate smoke -- though steam may be omitted;
c. Stacks to be fitted with grit arreaters;
snip...
1.2 Visual Imact
It is considered that the requirement for any carcase incinerator disign would be to ensure that the operations relating to the reception, storage and decepitation of diseased carcasses must not be publicly visible and that any part of a carcase could not be removed or interfered with by animals or birds.
REPORT ON BOVINE CARCASE INCINERATION
IF GOD DEMANDED
full text;
http://web.archive.org/web/20090506021132/http://www.bseinquiry.gov.uk/files/yb/1989/04/03006001.pdf
http://web.archive.org/web/20040521230540/http://www.bseinquiry.gov.uk/files/yb/1989/04/03006001.pdf
BSE, KURU, DENTAL AND ___CUT ABRASIONS___ from gutting a deer perhaps;
snip...
since there was a suggestion that kuru had been transmitted through the gums and/or gum abrasions...
snip...
http://web.archive.org/web/20090506054217/http://www.bseinquiry.gov.uk/files/yb/1989/04/17005001.pdf
http://web.archive.org/web/20040625025306/http://www.bseinquiry.gov.uk/files/yb/1989/04/17005001.pdf
Summary of Conclusions on the Vulnerability of Groundwater to Contamination by BSE Prions at Thruxted Mill.
[PDF]BSE INQUIRY Statement of behalf of the Environment Agency ... File Format: PDF/Adobe Acrobat - View as HTML ... his Statement of March 1998 to the BSE Inquiry ... systems subject to regular or intermittent contamination by rapid movement of recharge water ... www.bse.org.uk/files/ws/s490.pdf
BSE INQUIRY
Statement of behalf of the Environment Agency Concerning Thruxted Mill By Mr C. P. Young Principal Hydrogeologist, Soil Waste and Groundwater Group WRc plc; Medmenham, Bucks
SUNDAY, NOVEMBER 3, 2013
Environmental Impact Statements; Availability, etc.: Animal Carcass Management [Docket No. APHIS-2013-0044]
Environmental Impact Statements; Availability, etc.: Animal Carcass Management This Notice document was issued by the Animal and Plant Health Inspection Service (APHIS)
BSE infectivity survives burial for five years with only limited spread
Robert A. SomervilleKaren FernieAllister SmithKeith BishopBen C. MaddisonKevin C. GoughEmail authorNora HunterEmail author
Open AccessOriginal Article
First Online: 24 February 2019
Abstract
The carcasses of animals infected with bovine spongiform encephalopathy (BSE), scrapie or chronic wasting disease (CWD) that remain in the environment (exposed or buried) may continue to act as reservoirs of infectivity. We conducted two experiments under near-field conditions to investigate the survival and dissemination of BSE infectivity after burial in a clay or sandy soil. BSE infectivity was either contained within a bovine skull or buried as an uncontained bolus of BSE-infected brain. Throughout the five-year period of the experiment, BSE infectivity was recovered in similar amounts from heads exhumed annually from both types of soil. Very low levels of infectivity were detected in the soil immediately surrounding the heads, but not in samples remote from them. Similarly, there was no evidence of significant lateral movement of infectivity from the buried bolus over 4 years although there was a little vertical movement in both directions. However, bioassay analysis of limited numbers of samples of rain water that had drained through the bolus clay lysimeter indicated that infectivity was present in filtrates. sPMCA analysis also detected low levels of PrPSc in the filtrates up to 25 months following burial, raising the concern that leakage of infectivity into ground water could occur. We conclude that transmissible spongiform encephalopathy infectivity is likely to survive burial for long periods of time, but not to migrate far from the site of burial unless a vector or rain water drainage transports it. Risk assessments of contaminated sites should take these findings into account.
snip...
snip...
Here, we have shown that high levels of TSE infectivity can, and probably in most circumstances do, survive in brain tissue underground for very long periods of time – at least five years in this case – without significant loss of TSE infectivity. For example, we found that high levels of TSE infectivity were readily detected in cattle skull contents at similar levels each year for five years. Data also showed only limited migration from the site of deposition; infectivity was present in limited samples at 25 cm distance from the burial site, and up to 20 cm above the site and 50 cm below it. However, PrPSc was detectable by sPMCA in extracts of filters through which had drained a proportion of the water eluting from a 42.4-m3 clay lysimeter. PrPSc-positive samples were found up to 25 months after the burial of the 301V bolus sample. These data confirmed limited bioassay data that found infectivity in a filter extract sample taken at 25 months, one of two samples analysed. These results suggest a risk of spread of infection into watercourses if burial sites are not contained properly.
Our studies did not test the wide variety of soil chemistries and environmental conditions that might be encountered by TSE infectivity when deposited into soil. Nevertheless, these results should be taken into account when considering the future use and possible remediation of sites where BSE infectivity has been deposited. It should be assumed that high levels of BSE remain even after many years.
172. Establishment of PrPCWD extraction and detection methods in the farm soil
Kyung Je Park, Hoo Chang Park, In Soon Roh, Hyo Jin Kim, Hae-Eun Kang and Hyun Joo Sohn Foreign Animal Disease Division, Animal and Plant Quarantine Agency, Gimcheon, Gyeongsangbuk-do, Korea
ABSTRACT
Introduction: Transmissible spongiform encephalopathy (TSE) is a fatal neurodegenerative disorder, which is so-called as prion diseases due to the causative agents (PrPSc). TSEs are believed to be due to the template-directed accumulation of disease-associated prion protein, generally designated PrPSc. Chronic wasting disease (CWD) is the prion disease that is known spread horizontally. CWD has confirmed last in Republic of Korea in 2016 since first outbreak of CWD in 2001. The environmental reservoirs mediate the transmission of this disease. The significant levels of infectivity have been detected in the saliva, urine, and faeces of TSE-infected animals. Soil can serve as a stable reservoir for infectious prion proteins. We found that PrPCWD can be extracted and detected in CWD contaminated soil which has kept at room temperature until 4 years after 0.001 ~ 1% CWD exposure and natural CWD-affected farm soil through PBS washing and sPMCAb.
Materials and Methods: Procedure of serial PMCAb. CWD contaminated soil which has kept at room temperature (RT) for 1 ~ 4 year after 0.001%~1% CWD brain homogenates exposure for 4 months collected 0.14 g. The soil was collected by the same method once of year until 4 year after stop CWD exposure. We had conducted the two steps. There are two kinds of 10 times washing step and one amplification step. The washing step was detached PrPSc from contaminated soil by strong vortex with maximum rpm. We harvest supernatant every time by 10 times. As the other washing step, the Washed soil was made by washing 10 times soil using slow rotator and then harvest resuspended PBS for removing large impurity material. Last step was prion amplification step for detection of PrPCWD in soil supernatant and the washed soil by sPMCAb. Normal brain homogenate (NBH) was prepared by homogenization of brains with glass dounce in 9 volumes of cold PBS with TritonX-100, 5 mM EDTA, 150 mM NaCl and 0.05% Digitonin (sigma) plus Complete mini protease inhibitors (Roche) to a final concentration of 5%(w/v) NBHs were centrifuged at 2000 g for 1 min, and supernatant removed and frozen at −70 C for use. CWD consisted of brain from natural case in Korea and was prepared as 10%(w/v) homogenate. Positive sample was diluted to a final dilution 1:1000 in NBH, with serial 3:7 dilutions in NBH. Sonication was performed with a Misonix 4000 sonicator with amplitude set to level 70, generating an average output of 160W with two teflon beads during each cycle. One round consisted of 56 cycles of 30 s of sonication followed 9 min 30 s of 37°C incubation. Western Blotting (WB) for PrPSc detection. The samples (20 µL) after each round of amplification were mixed with proteinase K (2 mg/ml) and incubated 37°C for 1 h. Samples were separated by SDS-PAGE and transferred onto PVDF membrane. After blocking, the membrane was incubated for 1 h with 1st antibody S1 anti rabbit serum (APQA, 1:3000) and developed with enhanced chemiluminescence detection system.
Results: We excluded from first to third supernatant in view of sample contamination. It was confirmed abnormal PrP amplification in all soil supernatants from fourth to tenth. From 0.01% to 1% contaminated washed soils were identified as abnormal prions. 0.001% contaminated washed soil did not show PrP specific band (Fig 1). The soil was collected by the same method once of year until 4 year after stop CWD exposure. After sPMCAb, there were no PrPCWD band in from second to fourth year 0.001% washed soil. but It was confirmed that the abnormal prion was amplified in the washing supernatant which was not amplified in the washed soil. we have decided to use soil supernatant for soil testing (Fig. 2). After third rounds of amplification, PrPSc signals observed in three out of four sites from CWD positive farm playground. No signals were observed in all soil samples from four CWD negative farm (Fig. 3). Conclusions: Our studies showed that PrPCWD persist in 0.001% CWD contaminated soil for at least 4 year and natural CWD-affected farm soil. When cervid reintroduced into CWD outbreak farm, the strict decontamination procedures of the infectious agent should be performed in the environment of CWD-affected cervid habitat.
===
186. Serial detection of hematogenous prions in CWD-infected deer
Amy V. Nalls, Erin E. McNulty, Nathaniel D. Denkers, Edward A. Hoover and Candace K. Mathiason Department of Microbiology, Immunology, and Pathology, Colorado State University, Fort Collins, CO, USA CONTACT Amy V. Nalls amy.nalls@colostate.edu
ABSTRACT
Blood contains the infectious agent associated with prion disease affecting several mammalian species, including humans, cervids, sheep, and cattle. It has been confirmed that sufficient prion agent is present in the blood of both symptomatic and asymptomatic carriers to initiate the amyloid templating and accumulation process that results in this fatal neurodegenerative disease. Yet, to date, the ability to detect blood-borne prions by in vitro methods remains difficult.
We have capitalized on blood samples collected from longitudinal chronic wasting disease (CWD) studies in the native white-tailed deer host to examine hematogenous prion load in blood collected minutes, days, weeks and months post exposure. Our work has focused on refinement of the amplification methods RT-QuIC and PMCA. We demonstrate enhanced in vitro detection of amyloid seeding activity (prions) in blood cell fractions harvested from deer orally-exposed to 300 ng CWD positive brain or saliva.
These findings permit assessment of the role hematogenous prions play in the pathogenesis of CWD and provide tools to assess the same for prion diseases of other mammalian species.
2019
let's review some recent science on the environmental effects of the exposure of the cwd tse prion, it's not pretty...
THE tse prion aka mad cow type disease is not your normal pathogen.
The TSE prion disease survives ashing to 600 degrees celsius, that’s around 1112 degrees farenheit.
you cannot cook the TSE prion disease out of meat.
you can take the ash and mix it with saline and inject that ash into a mouse, and the mouse will go down with TSE.
Prion Infected Meat-and-Bone Meal Is Still Infectious after Biodiesel Production as well.
the TSE prion agent also survives Simulated Wastewater Treatment Processes.
IN fact, you should also know that the TSE Prion agent will survive in the environment for years, if not decades.
you can bury it and it will not go away.
The TSE agent is capable of infected your water table i.e. Detection of protease-resistant cervid prion protein in water from a CWD-endemic area.
it’s not your ordinary pathogen you can just cook it out and be done with.
***> that’s what’s so worrisome about Iatrogenic mode of transmission, a simple autoclave will not kill this TSE prion agent.
1: J Neurol Neurosurg Psychiatry 1994 Jun;57(6):757-8
***> Transmission of Creutzfeldt-Jakob disease to a chimpanzee by electrodes contaminated during neurosurgery.
Gibbs CJ Jr, Asher DM, Kobrine A, Amyx HL, Sulima MP, Gajdusek DC.
Laboratory of Central Nervous System Studies, National Institute of
Neurological Disorders and Stroke, National Institutes of Health,
Bethesda, MD 20892.
Stereotactic multicontact electrodes used to probe the cerebral cortex of a middle aged woman with progressive dementia were previously implicated in the accidental transmission of Creutzfeldt-Jakob disease (CJD) to two younger patients. The diagnoses of CJD have been confirmed for all three cases. More than two years after their last use in humans, after three cleanings and repeated sterilisation in ethanol and formaldehyde vapour, the electrodes were implanted in the cortex of a chimpanzee. Eighteen months later the animal became ill with CJD. This finding serves to re-emphasise the potential danger posed by reuse of instruments contaminated with the agents of spongiform encephalopathies, even after scrupulous attempts to clean them.
PMID: 8006664 [PubMed - indexed for MEDLINE]
P-147 Infection and detection of PrPCWD in soil from CWD infected farm in Korea
Hyun Joo Sohn, Kyung Je Park, In Soon Roh, Hyo Jin Kim, Hoo Chang Park, Byounghan Kim
Animal and Plant Quarantine Agency (QIA), Korea
Transmissible spongiform encephalopathy (TSE) is a fatal neurodegenerative disorder, which is so-called as prion diseases due to the causative agents (PrPSc). TSEs are believed to be due to the template-directed accumulation of disease-associated prion protein, generally designated PrPSc. Chronic wasting disease (CWD) is the prion disease that is known spread horizontally. CWD has confirmed last in Republic of Korea in 2010 since first outbreak of CWD in 2001. The environmental reservoirs mediate the transmission of this disease. The significant levels of infectivity have been detected in the saliva, urine, and feces of TSE-infected animals. Using serial protein misfolding cyclic amplification (sPMCA), we developed a detection method for CWD PrPSc in soil from CWD affected farm in 2010. We found to detect PrPSc in soil from CWD infected farm, but not detect PrPSc in soil of wild cervid habitats and normal cervid farm in Korea. We also tried the bioassay on transgenic mice overexpressing elk prion protein (TgElk mice) to confirm infectivity of CWD-infected farm soil and washing solution of it. As the results, there was the presence of infectious prions in them. The attack rates were each 12.5% (1/8, soil) and 100% (6/6, soil washing solution). Our method appears to be a very useful technique for monitoring PrPSc levels in environmental conditions.
Prion 2016 Conference Poster Abstracts
Prion 2016 Oral Abstracts
Prion 2016 Prion Diseases in Animals
Prion 2016 Prion Diseases in Humans
see full text;
PRION CONFERENCE 2019
172. Establishment of PrPCWD extraction and detection methods in the farm soil
Kyung Je Park, Hoo Chang Park, In Soon Roh, Hyo Jin Kim, Hae-Eun Kang and Hyun Joo Sohn
Foreign Animal Disease Division, Animal and Plant Quarantine Agency, Gimcheon, Gyeongsangbuk-do, Korea
ABSTRACT
Introduction: Transmissible spongiform encephalopathy (TSE) is a fatal neurodegenerative disorder, which is so-called as prion diseases due to the causative agents (PrPSc). TSEs are believed to be due to the template-directed accumulation of disease-associated prion protein, generally designated PrPSc. Chronic wasting disease (CWD) is the prion disease that is known spread horizontally. CWD has confirmed last in Republic of Korea in 2016 since first outbreak of CWD in 2001. The environmental reservoirs mediate the transmission of this disease. The significant levels of infectivity have been detected in the saliva, urine, and faeces of TSE-infected animals. Soil can serve as a stable reservoir for infectious prion proteins. We found that PrPCWD can be extracted and detected in CWD contaminated soil which has kept at room temperature until 4 years after 0.001 ~ 1% CWD exposure and natural CWD-affected farm soil through PBS washing and sPMCAb.
Materials and Methods: Procedure of serial PMCAb. CWD contaminated soil which has kept at room temperature (RT) for 1 ~ 4 year after 0.001%~1% CWD brain homogenates exposure for 4 months collected 0.14 g. The soil was collected by the same method once of year until 4 year after stop CWD exposure. We had conducted the two steps. There are two kinds of 10 times washing step and one amplification step. The washing step was detached PrPSc from contaminated soil by strong vortex with maximum rpm. We harvest supernatant every time by 10 times. As the other washing step, the Washed soil was made by washing 10 times soil using slow rotator and then harvest resuspended PBS for removing large impurity material. Last step was prion amplification step for detection of PrPCWD in soil supernatant and the washed soil by sPMCAb. Normal brain homogenate (NBH) was prepared by homogenization of brains with glass dounce in 9 volumes of cold PBS with TritonX-100, 5 mM EDTA, 150 mM NaCl and 0.05% Digitonin (sigma) plus Complete mini protease inhibitors (Roche) to a final concentration of 5%(w/v) NBHs were centrifuged at 2000 g for 1 min, and supernatant removed and frozen at −70 C for use. CWD consisted of brain from natural case in Korea and was prepared as 10%(w/v) homogenate. Positive sample was diluted to a final dilution 1:1000 in NBH, with serial 3:7 dilutions in NBH. Sonication was performed with a Misonix 4000 sonicator with amplitude set to level 70, generating an average output of 160W with two teflon beads during each cycle. One round consisted of 56 cycles of 30 s of sonication followed 9 min 30 s of 37°C incubation. Western Blotting (WB) for PrPSc detection. The samples (20 µL) after each round of amplification were mixed with proteinase K (2 mg/ml) and incubated 37°C for 1 h. Samples were separated by SDS-PAGE and transferred onto PVDF membrane. After blocking, the membrane was incubated for 1 h with 1st antibody S1 anti rabbit serum (APQA, 1:3000) and developed with enhanced chemiluminescence detection system.
Results: We excluded from first to third supernatant in view of sample contamination. It was confirmed abnormal PrP amplification in all soil supernatants from fourth to tenth. From 0.01% to 1% contaminated washed soils were identified as abnormal prions. 0.001% contaminated washed soil did not show PrP specific band (Fig 1). The soil was collected by the same method once of year until 4 year after stop CWD exposure. After sPMCAb, there were no PrPCWD band in from second to fourth year 0.001% washed soil. but It was confirmed that the abnormal prion was amplified in the washing supernatant which was not amplified in the washed soil. we have decided to use soil supernatant for soil testing (Fig. 2). After third rounds of amplification, PrPSc signals observed in three out of four sites from CWD positive farm playground. No signals were observed in all soil samples from four CWD negative farm (Fig. 3).
Conclusions: Our studies showed that PrPCWD persist in 0.001% CWD contaminated soil for at least 4 year and natural CWD-affected farm soil. When cervid reintroduced into CWD outbreak farm, the strict decontamination procedures of the infectious agent should be performed in the environment of CWD-affected cervid habitat.
2018 - 2019
***> This is very likely to have parallels with control efforts for CWD in cervids.
Rapid recontamination of a farm building occurs after attempted prion removal
Kevin Christopher Gough, BSc (Hons), PhD1, Claire Alison Baker, BSc (Hons)2, Steve Hawkins, MIBiol3, Hugh Simmons, BVSc, MRCVS, MBA, MA3, Timm Konold, DrMedVet, PhD, MRCVS3 and Ben Charles Maddison, BSc (Hons), PhD2
Abstract
The transmissible spongiform encephalopathy scrapie of sheep/goats and chronic wasting disease of cervids are associated with environmental reservoirs of infectivity.
Preventing environmental prions acting as a source of infectivity to healthy animals is of major concern to farms that have had outbreaks of scrapie and also to the health management of wild and farmed cervids.
Here, an efficient scrapie decontamination protocol was applied to a farm with high levels of environmental contamination with the scrapie agent.
Post-decontamination, no prion material was detected within samples taken from the farm buildings as determined using a sensitive in vitro replication assay (sPMCA).
A bioassay consisting of 25 newborn lambs of highly susceptible prion protein genotype VRQ/VRQ introduced into this decontaminated barn was carried out in addition to sampling and analysis of dust samples that were collected during the bioassay.
Twenty-four of the animals examined by immunohistochemical analysis of lymphatic tissues were scrapie-positive during the bioassay, samples of dust collected within the barn were positive by month 3.
The data illustrates the difficulty in decontaminating farm buildings from scrapie, and demonstrates the likely contribution of farm dust to the recontamination of these environments to levels that are capable of causing disease.
snip...
As in the authors' previous study,12 the decontamination of this sheep barn was not effective at removing scrapie infectivity, and despite the extra measures brought into this study (more effective chemical treatment and removal of sources of dust) the overall rates of disease transmission mirror previous results on this farm. With such apparently effective decontamination (assuming that at least some sPMCA seeding ability is coincident with infectivity), how was infectivity able to persist within the environment and where does infectivity reside? Dust samples were collected in both the bioassay barn and also a barn subject to the same decontamination regime within the same farm (but remaining unoccupied). Within both of these barns dust had accumulated for three months that was able to seed sPMCA, indicating the accumulation of scrapie-containing material that was independent of the presence of sheep that may have been incubating and possibly shedding low amounts of infectivity.
This study clearly demonstrates the difficulty in removing scrapie infectivity from the farm environment. Practical and effective prion decontamination methods are still urgently required for decontamination of scrapie infectivity from farms that have had cases of scrapie and this is particularly relevant for scrapiepositive goatherds, which currently have limited genetic resistance to scrapie within commercial breeds.24 This is very likely to have parallels with control efforts for CWD in cervids.
Acknowledgements The authors thank the APHA farm staff, Tony Duarte, Olly Roberts and Margaret Newlands for preparation of the sheep pens and animal husbandry during the study. The authors also thank the APHA pathology team for RAMALT and postmortem examination.
Funding This study was funded by DEFRA within project SE1865.
Competing interests None declared.
Saturday, January 5, 2019
Rapid recontamination of a farm building occurs after attempted prion removal
THURSDAY, FEBRUARY 28, 2019
BSE infectivity survives burial for five years with only limited spread
***> CONGRESSIONAL ABSTRACTS PRION CONFERENCE 2018
P69 Experimental transmission of CWD from white-tailed deer to co-housed reindeer
Mitchell G (1), Walther I (1), Staskevicius A (1), Soutyrine A (1), Balachandran A (1)
(1) National & OIE Reference Laboratory for Scrapie and CWD, Canadian Food Inspection Agency, Ottawa, Ontario, Canada.
Chronic wasting disease (CWD) continues to be detected in wild and farmed cervid populations of North America, affecting predominantly white-tailed deer, mule deer and elk. Extensive herds of wild caribou exist in northern regions of Canada, although surveillance has not detected the presence of CWD in this population. Oral experimental transmission has demonstrated that reindeer, a species closely related to caribou, are susceptible to CWD. Recently, CWD was detected for the first time in Europe, in wild Norwegian reindeer, advancing the possibility that caribou in North America could also become infected. Given the potential overlap in habitat between wild CWD-infected cervids and wild caribou herds in Canada, we sought to investigate the horizontal transmissibility of CWD from white-tailed deer to reindeer.
Two white-tailed deer were orally inoculated with a brain homogenate prepared from a farmed Canadian white-tailed deer previously diagnosed with CWD. Two reindeer, with no history of exposure to CWD, were housed in the same enclosure as the white-tailed deer, 3.5 months after the deer were orally inoculated. The white-tailed deer developed clinical signs consistent with CWD beginning at 15.2 and 21 months post-inoculation (mpi), and were euthanized at 18.7 and 23.1 mpi, respectively. Confirmatory testing by immunohistochemistry (IHC) and western blot demonstrated widespread aggregates of pathological prion protein (PrPCWD) in the central nervous system and lymphoid tissues of both inoculated white-tailed deer. Both reindeer were subjected to recto-anal mucosal associated lymphoid tissue (RAMALT) biopsy at 20 months post-exposure (mpe) to the white-tailed deer. The biopsy from one reindeer contained PrPCWD confirmed by IHC. This reindeer displayed only subtle clinical evidence of disease prior to a rapid decline in condition requiring euthanasia at 22.5 mpe. Analysis of tissues from this reindeer by IHC revealed widespread PrPCWD deposition, predominantly in central nervous system and lymphoreticular tissues. Western blot molecular profiles were similar between both orally inoculated white-tailed deer and the CWD positive reindeer. Despite sharing the same enclosure, the other reindeer was RAMALT negative at 20 mpe, and PrPCWD was not detected in brainstem and lymphoid tissues following necropsy at 35 mpe. Sequencing of the prion protein gene from both reindeer revealed differences at several codons, which may have influenced susceptibility to infection.
Natural transmission of CWD occurs relatively efficiently amongst cervids, supporting the expanding geographic distribution of disease and the potential for transmission to previously naive populations. The efficient horizontal transmission of CWD from white-tailed deer to reindeer observed here highlights the potential for reindeer to become infected if exposed to other cervids or environments infected with CWD.
***> Infectious agent of sheep scrapie may persist in the environment for at least 16 years
***> Nine of these recurrences occurred 14–21 years after culling, apparently as the result of environmental contamination, but outside entry could not always be absolutely excluded.
Gudmundur Georgsson,1 Sigurdur Sigurdarson2 and Paul Brown3
Correspondence
Gudmundur Georgsson ggeorgs@hi.is
1 Institute for Experimental Pathology, University of Iceland, Keldur v/vesturlandsveg, IS-112 Reykjavı´k, Iceland
2 Laboratory of the Chief Veterinary Officer, Keldur, Iceland
3 Bethesda, Maryland, USA
Received 7 March 2006 Accepted 6 August 2006
In 1978, a rigorous programme was implemented to stop the spread of, and subsequently eradicate, sheep scrapie in Iceland. Affected flocks were culled, premises were disinfected and, after 2–3 years, restocked with lambs from scrapie-free areas. Between 1978 and 2004, scrapie recurred on 33 farms. Nine of these recurrences occurred 14–21 years after culling, apparently as the result of environmental contamination, but outside entry could not always be absolutely excluded. Of special interest was one farm with a small, completely self-contained flock where scrapie recurred 18 years after culling, 2 years after some lambs had been housed in an old sheephouse that had never been disinfected. Epidemiological investigation established with near certitude that the disease had not been introduced from the outside and it is concluded that the agent may have persisted in the old sheep-house for at least 16 years.
TITLE: PATHOLOGICAL FEATURES OF CHRONIC WASTING DISEASE IN REINDEER AND DEMONSTRATION OF HORIZONTAL TRANSMISSION
*** DECEMBER 2016 CDC EMERGING INFECTIOUS DISEASE JOURNAL CWD HORIZONTAL TRANSMISSION
SEE;
Back around 2000, 2001, or so, I was corresponding with officials abroad during the bse inquiry, passing info back and forth, and some officials from here inside USDA aphis FSIS et al. In fact helped me get into the USA 50 state emergency BSE conference call way back. That one was a doozy. But I always remember what “deep throat” I never knew who they were, but I never forgot;
Some unofficial information from a source on the inside looking out -
Confidential!!!!
As early as 1992-3 there had been long studies conducted on small pastures containing scrapie infected sheep at the sheep research station associated with the Neuropathogenesis Unit in Edinburgh, Scotland. Whether these are documented...I don't know. But personal recounts both heard and recorded in a daily journal indicate that leaving the pastures free and replacing the topsoil completely at least 2 feet of thickness each year for SEVEN years....and then when very clean (proven scrapie free) sheep were placed on these small pastures.... the new sheep also broke out with scrapie and passed it to offspring. I am not sure that TSE contaminated ground could ever be free of the agent!! A very frightening revelation!!!
---end personal email---end...tss
Infectivity surviving ashing to 600*C is (in my opinion) degradable but infective. based on Bown & Gajdusek, (1991), landfill and burial may be assumed to have a reduction factor of 98% (i.e. a factor of 50) over 3 years. CJD-infected brain-tissue remained infectious after storing at room-temperature for 22 months (Tateishi et al, 1988). Scrapie agent is known to remain viable after at least 30 months of desiccation (Wilson et al, 1950). and pastures that had been grazed by scrapie-infected sheep still appeared to be contaminated with scrapie agent three years after they were last occupied by sheep (Palsson, 1979).
Dr. Paul Brown Scrapie Soil Test BSE Inquiry Document
Using in vitro Prion replication for high sensitive detection of prions and prionlike proteins and for understanding mechanisms of transmission.
Claudio Soto Mitchell Center for Alzheimer's diseases and related Brain disorders, Department of Neurology, University of Texas Medical School at Houston.
Prion and prion-like proteins are misfolded protein aggregates with the ability to selfpropagate to spread disease between cells, organs and in some cases across individuals. I n T r a n s m i s s i b l e s p o n g i f o r m encephalopathies (TSEs), prions are mostly composed by a misfolded form of the prion protein (PrPSc), which propagates by transmitting its misfolding to the normal prion protein (PrPC). The availability of a procedure to replicate prions in the laboratory may be important to study the mechanism of prion and prion-like spreading and to develop high sensitive detection of small quantities of misfolded proteins in biological fluids, tissues and environmental samples. Protein Misfolding Cyclic Amplification (PMCA) is a simple, fast and efficient methodology to mimic prion replication in the test tube. PMCA is a platform technology that may enable amplification of any prion-like misfolded protein aggregating through a seeding/nucleation process. In TSEs, PMCA is able to detect the equivalent of one single molecule of infectious PrPSc and propagate prions that maintain high infectivity, strain properties and species specificity. Using PMCA we have been able to detect PrPSc in blood and urine of experimentally infected animals and humans affected by vCJD with high sensitivity and specificity. Recently, we have expanded the principles of PMCA to amplify amyloid-beta (Aβ) and alphasynuclein (α-syn) aggregates implicated in Alzheimer's and Parkinson's diseases, respectively. Experiments are ongoing to study the utility of this technology to detect Aβ and α-syn aggregates in samples of CSF and blood from patients affected by these diseases.
=========================
***>>> Recently, we have been using PMCA to study the role of environmental prion contamination on the horizontal spreading of TSEs. These experiments have focused on the study of the interaction of prions with plants and environmentally relevant surfaces. Our results show that plants (both leaves and roots) bind tightly to prions present in brain extracts and excreta (urine and feces) and retain even small quantities of PrPSc for long periods of time. Strikingly, ingestion of prioncontaminated leaves and roots produced disease with a 100% attack rate and an incubation period not substantially longer than feeding animals directly with scrapie brain homogenate. Furthermore, plants can uptake prions from contaminated soil and transport them to different parts of the plant tissue (stem and leaves). Similarly, prions bind tightly to a variety of environmentally relevant surfaces, including stones, wood, metals, plastic, glass, cement, etc. Prion contaminated surfaces efficiently transmit prion disease when these materials were directly injected into the brain of animals and strikingly when the contaminated surfaces were just placed in the animal cage. These findings demonstrate that environmental materials can efficiently bind infectious prions and act as carriers of infectivity, suggesting that they may play an important role in the horizontal transmission of the disease.
========================
Since its invention 13 years ago, PMCA has helped to answer fundamental questions of prion propagation and has broad applications in research areas including the food industry, blood bank safety and human and veterinary disease diagnosis.
New studies on the heat resistance of hamster-adapted scrapie agent: Threshold survival after ashing at 600°C suggests an inorganic template of replication
Prion Infected Meat-and-Bone Meal Is Still Infectious after Biodiesel Production
Detection of protease-resistant cervid prion protein in water from a CWD-endemic area
A Quantitative Assessment of the Amount of Prion Diverted to Category 1 Materials and Wastewater During Processing
Rapid assessment of bovine spongiform encephalopathy prion inactivation by heat treatment in yellow grease produced in the industrial manufacturing process of meat and bone meals
PPo4-4:
Survival and Limited Spread of TSE Infectivity after Burial
Discussion Classical scrapie is an environmentally transmissible disease because it has been reported in naïve, supposedly previously unexposed sheep placed in pastures formerly occupied by scrapie-infected sheep (4, 19, 20).
Although the vector for disease transmission is not known, soil is likely to be an important reservoir for prions (2) where – based on studies in rodents – prions can adhere to minerals as a biologically active form (21) and remain infectious for more than 2 years (22).
Similarly, chronic wasting disease (CWD) has re-occurred in mule deer housed in paddocks used by infected deer 2 years earlier, which was assumed to be through foraging and soil consumption (23).
Our study suggested that the risk of acquiring scrapie infection was greater through exposure to contaminated wooden, plastic, and metal surfaces via water or food troughs, fencing, and hurdles than through grazing.
Drinking from a water trough used by the scrapie flock was sufficient to cause infection in sheep in a clean building.
Exposure to fences and other objects used for rubbing also led to infection, which supported the hypothesis that skin may be a vector for disease transmission (9).
The risk of these objects to cause infection was further demonstrated when 87% of 23 sheep presented with PrPSc in lymphoid tissue after grazing on one of the paddocks, which contained metal hurdles, a metal lamb creep and a water trough in contact with the scrapie flock up to 8 weeks earlier, whereas no infection had been demonstrated previously in sheep grazing on this paddock, when equipped with new fencing and field furniture.
When the contaminated furniture and fencing were removed, the infection rate dropped significantly to 8% of 12 sheep, with soil of the paddock as the most likely source of infection caused by shedding of prions from the scrapie-infected sheep in this paddock up to a week earlier.
This study also indicated that the level of contamination of field furniture sufficient to cause infection was dependent on two factors: stage of incubation period and time of last use by scrapie-infected sheep.
Drinking from a water trough that had been used by scrapie sheep in the predominantly pre-clinical phase did not appear to cause infection, whereas infection was shown in sheep drinking from the water trough used by scrapie sheep in the later stage of the disease.
It is possible that contamination occurred through shedding of prions in saliva, which may have contaminated the surface of the water trough and subsequently the water when it was refilled.
Contamination appeared to be sufficient to cause infection only if the trough was in contact with sheep that included clinical cases.
Indeed, there is an increased risk of bodily fluid infectivity with disease progression in scrapie (24) and CWD (25) based on PrPSc detection by sPMCA.
Although ultraviolet light and heat under natural conditions do not inactivate prions (26), furniture in contact with the scrapie flock, which was assumed to be sufficiently contaminated to cause infection, did not act as vector for disease if not used for 18 months, which suggest that the weathering process alone was sufficient to inactivate prions.
PrPSc detection by sPMCA is increasingly used as a surrogate for infectivity measurements by bioassay in sheep or mice.
In this reported study, however, the levels of PrPSc present in the environment were below the limit of detection of the sPMCA method, yet were still sufficient to cause infection of in-contact animals.
In the present study, the outdoor objects were removed from the infected flock 8 weeks prior to sampling and were positive by sPMCA at very low levels (2 out of 37 reactions).
As this sPMCA assay also yielded 2 positive reactions out of 139 in samples from the scrapie-free farm, the sPMCA assay could not detect PrPSc on any of the objects above the background of the assay.
False positive reactions with sPMCA at a low frequency associated with de novo formation of infectious prions have been reported (27, 28).
This is in contrast to our previous study where we demonstrated that outdoor objects that had been in contact with the scrapie-infected flock up to 20 days prior to sampling harbored PrPSc that was detectable by sPMCA analysis [4 out of 15 reactions (12)] and was significantly more positive by the assay compared to analogous samples from the scrapie-free farm.
This discrepancy could be due to the use of a different sPMCA substrate between the studies that may alter the efficiency of amplification of the environmental PrPSc.
In addition, the present study had a longer timeframe between the objects being in contact with the infected flock and sampling, which may affect the levels of extractable PrPSc.
Alternatively, there may be potentially patchy contamination of this furniture with PrPSc, which may have been missed by swabbing.
The failure of sPMCA to detect CWD-associated PrP in saliva from clinically affected deer despite confirmation of infectivity in saliva-inoculated transgenic mice was associated with as yet unidentified inhibitors in saliva (29), and it is possible that the sensitivity of sPMCA is affected by other substances in the tested material.
In addition, sampling of amplifiable PrPSc and subsequent detection by sPMCA may be more difficult from furniture exposed to weather, which is supported by the observation that PrPSc was detected by sPMCA more frequently in indoor than outdoor furniture (12).
A recent experimental study has demonstrated that repeated cycles of drying and wetting of prion-contaminated soil, equivalent to what is expected under natural weathering conditions, could reduce PMCA amplification efficiency and extend the incubation period in hamsters inoculated with soil samples (30).
This seems to apply also to this study even though the reduction in infectivity was more dramatic in the sPMCA assays than in the sheep model.
Sheep were not kept until clinical end-point, which would have enabled us to compare incubation periods, but the lack of infection in sheep exposed to furniture that had not been in contact with scrapie sheep for a longer time period supports the hypothesis that prion degradation and subsequent loss of infectivity occurs even under natural conditions.
In conclusion, the results in the current study indicate that removal of furniture that had been in contact with scrapie-infected animals should be recommended, particularly since cleaning and decontamination may not effectively remove scrapie infectivity (31), even though infectivity declines considerably if the pasture and the field furniture have not been in contact with scrapie-infected sheep for several months. As sPMCA failed to detect PrPSc in furniture that was subjected to weathering, even though exposure led to infection in sheep, this method may not always be reliable in predicting the risk of scrapie infection through environmental contamination.
These results suggest that the VRQ/VRQ sheep model may be more sensitive than sPMCA for the detection of environmentally associated scrapie, and suggest that extremely low levels of scrapie contamination are able to cause infection in susceptible sheep genotypes.
Keywords: classical scrapie, prion, transmissible spongiform encephalopathy, sheep, field furniture, reservoir, serial protein misfolding cyclic amplification
Wednesday, December 16, 2015
*** Objects in contact with classical scrapie sheep act as a reservoir for scrapie transmission ***
TUESDAY, OCTOBER 01, 2019
Genetic susceptibility to chronic wasting disease cwd tse prion?
i am concerned with the fact, the longer you can delay death with cwd, you risk having a cwd tse prion infected deer live longer in the wild or captive, thus giving more time to spread disease. you also risk developing a super cwd tse strain imo. we already have multiple strains, with what seems to be a super strain of cwd in Texas. also, with scrapie, they thought arr was resistant in sheep, until it was not...
Colorado Chronic Wasting Disease Response Plan December 2018
I. Executive Summary Mule deer, white-tailed deer, elk and moose are highly valued species in North America. Some of Colorado’s herds of these species are increasingly becoming infected with chronic wasting disease (CWD). As of July 2018, at least 31 of Colorado's 54 deer herds (57%), 16 of 43 elk herds (37%), and 2 of 9 moose herds (22%) are known to be infected with CWD. Four of Colorado's 5 largest deer herds and 2 of the state’s 5 largest elk herds are infected. Deer herds tend to be more heavily infected than elk and moose herds living in the same geographic area. Not only are the number of infected herds increasing, the past 15 years of disease trends generally show an increase in the proportion of infected animals within herds as well. Of most concern, greater than a 10-fold increase in CWD prevalence has been estimated in some mule deer herds since the early 2000s; CWD is now adversely affecting the performance of these herds.
snip...
(the map on page 71, cwd marked in red, is shocking...tss)
ZOONOSIS OF CWD, BSE, SCRAPIE, TSE PRION
CWD TSE Prion Zoonosis
i was very surprised that no mention of the study out of Canada with oral transmission of CWD to Macaque.
i have spoken with Stefanie Czub and Professor Aguzzi, whom toured her lab afterwards, about these studies. the transmission studies were valid. plus, we know that cwd zoonosis would NOT look like nvCJD, but would look like sporadic CJD of some type. see;
> However, to date, no CWD infections have been reported in people.
key word here is ‘reported’. science has shown that CWD in humans will look like sporadic CJD. SO, how can one assume that CWD has not already transmitted to humans? they can’t, and it’s as simple as that. from all recorded science to date, CWD has already transmitted to humans, and it’s being misdiagnosed as sporadic CJD. …terry
*** LOOKING FOR CWD IN HUMANS AS nvCJD or as an ATYPICAL CJD, LOOKING IN ALL THE WRONG PLACES $$$ ***
*** These results would seem to suggest that CWD does indeed have zoonotic potential, at least as judged by the compatibility of CWD prions and their human PrPC target. Furthermore, extrapolation from this simple in vitro assay suggests that if zoonotic CWD occurred, it would most likely effect those of the PRNP codon 129-MM genotype and that the PrPres type would be similar to that found in the most common subtype of sCJD (MM1).***
Chronic Wasting Disease CWD TSE Prion aka mad deer disease zoonosis
We hypothesize that:
(1) The classic CWD prion strain can infect humans at low levels in the brain and peripheral lymphoid tissues;
(2) The cervid-to-human transmission barrier is dependent on the cervid prion strain and influenced by the host (human) prion protein (PrP) primary sequence;
(3) Reliable essays can be established to detect CWD infection in humans; and
(4) CWD transmission to humans has already occurred. We will test these hypotheses in 4 Aims using transgenic (Tg) mouse models and complementary in vitro approaches.
ZOONOTIC CHRONIC WASTING DISEASE CWD TSE PRION UPDATE
Prion 2017 Conference
First evidence of intracranial and peroral transmission of Chronic Wasting Disease (CWD) into Cynomolgus macaques: a work in progress Stefanie Czub1, Walter Schulz-Schaeffer2, Christiane Stahl-Hennig3, Michael Beekes4, Hermann Schaetzl5 and Dirk Motzkus6 1
University of Calgary Faculty of Veterinary Medicine/Canadian Food Inspection Agency; 2Universitatsklinikum des Saarlandes und Medizinische Fakultat der Universitat des Saarlandes; 3 Deutsches Primaten Zentrum/Goettingen; 4 Robert-Koch-Institut Berlin; 5 University of Calgary Faculty of Veterinary Medicine; 6 presently: Boehringer Ingelheim Veterinary Research Center; previously: Deutsches Primaten Zentrum/Goettingen
This is a progress report of a project which started in 2009. 21 cynomolgus macaques were challenged with characterized CWD material from white-tailed deer (WTD) or elk by intracerebral (ic), oral, and skin exposure routes. Additional blood transfusion experiments are supposed to assess the CWD contamination risk of human blood product. Challenge materials originated from symptomatic cervids for ic, skin scarification and partially per oral routes (WTD brain). Challenge material for feeding of muscle derived from preclinical WTD and from preclinical macaques for blood transfusion experiments. We have confirmed that the CWD challenge material contained at least two different CWD agents (brain material) as well as CWD prions in muscle-associated nerves.
Here we present first data on a group of animals either challenged ic with steel wires or per orally and sacrificed with incubation times ranging from 4.5 to 6.9 years at postmortem. Three animals displayed signs of mild clinical disease, including anxiety, apathy, ataxia and/or tremor. In four animals wasting was observed, two of those had confirmed diabetes. All animals have variable signs of prion neuropathology in spinal cords and brains and by supersensitive IHC, reaction was detected in spinal cord segments of all animals. Protein misfolding cyclic amplification (PMCA), real-time quaking-induced conversion (RT-QuiC) and PET-blot assays to further substantiate these findings are on the way, as well as bioassays in bank voles and transgenic mice.
At present, a total of 10 animals are sacrificed and read-outs are ongoing. Preclinical incubation of the remaining macaques covers a range from 6.4 to 7.10 years. Based on the species barrier and an incubation time of > 5 years for BSE in macaques and about 10 years for scrapie in macaques, we expected an onset of clinical disease beyond 6 years post inoculation.
PRION 2017 DECIPHERING NEURODEGENERATIVE DISORDERS
PRION 2018 CONFERENCE
Oral transmission of CWD into Cynomolgus macaques: signs of atypical disease, prion conversion and infectivity in macaques and bio-assayed transgenic mice
Hermann M. Schatzl, Samia Hannaoui, Yo-Ching Cheng, Sabine Gilch (Calgary Prion Research Unit, University of Calgary, Calgary, Canada) Michael Beekes (RKI Berlin), Walter Schulz-Schaeffer (University of Homburg/Saar, Germany), Christiane Stahl-Hennig (German Primate Center) & Stefanie Czub (CFIA Lethbridge).
To date, BSE is the only example of interspecies transmission of an animal prion disease into humans. The potential zoonotic transmission of CWD is an alarming issue and was addressed by many groups using a variety of in vitro and in vivo experimental systems. Evidence from these studies indicated a substantial, if not absolute, species barrier, aligning with the absence of epidemiological evidence suggesting transmission into humans. Studies in non-human primates were not conclusive so far, with oral transmission into new-world monkeys and no transmission into old-world monkeys. Our consortium has challenged 18 Cynomolgus macaques with characterized CWD material, focusing on oral transmission with muscle tissue. Some macaques have orally received a total of 5 kg of muscle material over a period of 2 years.
After 5-7 years of incubation time some animals showed clinical symptoms indicative of prion disease, and prion neuropathology and PrPSc deposition were detected in spinal cord and brain of some euthanized animals. PrPSc in immunoblot was weakly detected in some spinal cord materials and various tissues tested positive in RT-QuIC, including lymph node and spleen homogenates. To prove prion infectivity in the macaque tissues, we have intracerebrally inoculated 2 lines of transgenic mice, expressing either elk or human PrP. At least 3 TgElk mice, receiving tissues from 2 different macaques, showed clinical signs of a progressive prion disease and brains were positive in immunoblot and RT-QuIC. Tissues (brain, spinal cord and spleen) from these and pre-clinical mice are currently tested using various read-outs and by second passage in mice. Transgenic mice expressing human PrP were so far negative for clear clinical prion disease (some mice >300 days p.i.). In parallel, the same macaque materials are inoculated into bank voles.
Taken together, there is strong evidence of transmissibility of CWD orally into macaques and from macaque tissues into transgenic mouse models, although with an incomplete attack rate.
The clinical and pathological presentation in macaques was mostly atypical, with a strong emphasis on spinal cord pathology.
Our ongoing studies will show whether the transmission of CWD into macaques and passage in transgenic mice represents a form of non-adaptive prion amplification, and whether macaque-adapted prions have the potential to infect mice expressing human PrP.
Our ongoing studies will show whether the transmission of CWD into macaques and passage in transgenic mice represents a form of non-adaptive prion amplification, and whether macaque-adapted prions have the potential to infect mice expressing human PrP.
The notion that CWD can be transmitted orally into both new-world and old-world non-human primates asks for a careful reevaluation of the zoonotic risk of CWD..
***> The notion that CWD can be transmitted orally into both new-world and old-world non-human primates asks for a careful reevaluation of the zoonotic risk of CWD. <***
READING OVER THE PRION 2018 ABSTRACT BOOK, LOOKS LIKE THEY FOUND THAT from this study ;
P190 Human prion disease mortality rates by occurrence of chronic wasting disease in freeranging cervids, United States
Abrams JY (1), Maddox RA (1), Schonberger LB (1), Person MK (1), Appleby BS (2), Belay ED (1) (1) Centers for Disease Control and Prevention (CDC), National Center for Emerging and Zoonotic Infectious Diseases, Atlanta, GA, USA (2) Case Western Reserve University, National Prion Disease Pathology Surveillance Center (NPDPSC), Cleveland, OH, USA..
SEEMS THAT THEY FOUND Highly endemic states had a higher rate of prion disease mortality compared to non-CWD
states.
states.
AND ANOTHER STUDY;
P172 Peripheral Neuropathy in Patients with Prion Disease
Wang H(1), Cohen M(1), Appleby BS(1,2) (1) University Hospitals Cleveland Medical Center, Cleveland, Ohio (2) National Prion Disease Pathology Surveillance Center, Cleveland, Ohio..
IN THIS STUDY, THERE WERE autopsy-proven prion cases from the National Prion Disease Pathology Surveillance Center that were diagnosed between September 2016 to March 2017,
AND
included 104 patients. SEEMS THEY FOUND THAT The most common sCJD subtype was MV1-2 (30%), followed by MM1-2 (20%),
AND
THAT The Majority of cases were male (60%), AND half of them had exposure to wild game.
snip…
see more on Prion 2017 Macaque study from Prion 2017 Conference and other updated science on cwd tse prion zoonosis below…terry
PRION 2019 ABSTRACTS
1. Interspecies transmission of the chronic wasting disease agent
Justin Greenlee
Virus and Prion Research Unit, National Animal Disease Center, USDA Agriculture Research Service
ABSTRACT
The presentation will summarize the results of various studies conducted at our research center that assess the transmissibility of the chronic wasting disease (CWD) agent to cattle, pigs, raccoons, goats, and sheep. This will include specifics of the relative attack rates, clinical signs, and microscopic lesions with emphasis on how to differentiate cross-species transmission of the CWD agent from the prion diseases that naturally occur in hosts such as cattle or sheep. Briefly, the relative difficulty of transmitting the CWD agent to sheep and goats will be contrasted with the relative ease of transmitting the scrapie agent to white-tailed deer.
53. Evaluation of the inter-species transmission potential of different CWD isolates
Rodrigo Moralesa, Carlos Kramma,b, Paulina Sotoa, Adam Lyona, Sandra Pritzkowa, Claudio Sotoa
aMitchell Center for Alzheimer’s disease and Related Brain Disorders, Dept. of Neurology, McGovern School of Medicine University of Texas Health Science Center at Houston, TX, USA; bFacultad de Medicina, Universidad de los Andes, Santiago, Chile
ABSTRACT
Chronic Wasting Disease (CWD) has reached epidemic proportions in North America and has been identified in South Korea and Northern Europe. CWD-susceptible cervid species are known to share habitats with humans and other animals entering the human food chain. At present, the potential of CWD to infect humans and other animal species is not completely clear. The exploration of this issue acquires further complexity considering the differences in the prion protein sequence due to species-specific variations and polymorphic changes within species. While several species of cervids are naturally affected by CWD, white-tailed deer (WTD) is perhaps the most relevant due to its extensive use in hunting and as a source of food. Evaluation of inter-species prion infections using animals or mouse models is costly and time consuming. We and others have shown that the Protein Misfolding Cyclic Amplification (PMCA) technology reproduces, in an accelerated and inexpensive manner, the inter-species transmission of prions while preserving the strain features of the input PrPSc. In this work, we tested the potential of different WTD-derived CWD isolates to transmit to humans and other animal species relevant for human consumption using PMCA. For these experiments, CWD isolates homozygous for the most common WTD-PrP polymorphic changes (G96S) were used (96SS variant obtained from a pre-symptomatic prion infected WTD). Briefly, 96GG and 96SS CWD prions were adapted in homologous or heterologous substrate by PMCA through several (15) rounds. End products, as well as intermediates across the process, were tested for their inter-species transmission potentials. A similar process was followed to assess seed-templated misfolding of ovine, porcine, and bovine PrPC. Our results show differences on the inter-species transmission potentials of the four adapted materials generated (PrPC/PrPSc polymorphic combinations), being the homologous combinations of seed/substrate the ones with the greater apparent zoonotic potential. Surprisingly, 96SS prions adapted in homologous substrate were the ones showing the easiest potential to template PrPC misfolding from other animal species. In summary, our results show that a plethora of different CWD isolates, each comprising different potentials for inter-species transmission, may exist in the environment. These experiments may help to clarify an uncertain and potentially worrisome public health issue. Additional research in this area may be useful to advise on the design of regulations intended to stop the spread of CWD and predict unwanted zoonotic events.
56. Understanding chronic wasting disease spread potential for at-risk species
Catherine I. Cullingham, Anh Dao, Debbie McKenzie and David W. Coltman
Department of Biological Sciences, University of Alberta, Edmonton AB, Canada
CONTACT Catherine I. Cullingham cathy.cullingham@ualberta.ca
ABSTRACT
Genetic variation can be linked to susceptibility or resistance to a disease, and this information can help to better understand spread-risk in a population. Wildlife disease incidence is increasing, and this is resulting in negative impacts on the economy, biodiversity, and in some instances, human health. If we can find genetic variation that helps to inform which individuals are susceptible, then we can use this information on at-risk populations to better manage negative consequences. Chronic wasting disease, a fatal, transmissible spongiform encephalopathy of cervids (both wild and captive), continues to spread geographically, which has resulted in an increasing host-range. The disease agent (PrPCWD) is a misfolded conformer of native cellular protein (PrPC). In Canada, the disease is endemic in Alberta and Saskatchewan, infecting primarily mule deer and white-tail deer, with a smaller impact on elk and moose populations. As the extent of the endemic area continues to expand, additional species will be exposed to this disease, including bison, bighorn sheep, mountain goat, and pronghorn antelope. To better understand the potential spread-risk among these species, we reviewed the current literature on species that have been orally exposed to CWD to identify susceptible and resistant species. We then compared the amino acid polymorphisms of PrPC among these species to determine whether any sites were linked to susceptibility or resistance to CWD infection. We sequenced the entire PrP coding region in 578 individuals across at-risk populations to evaluate their potential susceptibility. Three amino acid sites (97, 170, and 174; human numbering) were significantly associated with susceptibility, but these were not fully discriminating. All but one species among the resistant group shared the same haplotype, and the same for the susceptible species. For the at-risk species, bison had the resistant haplotype, while bighorn sheep and mountain goats were closely associated with the resistant type. Pronghorn antelope and a newly identified haplotype in moose differed from the susceptible haplotype, but were still closely associated with it. These data suggest pronghorn antelope will be susceptible to CWD while bison are likely to be resistant. Based on this data, recommendations can be made regarding species to be monitored for possible CWD infection.
KEYWORDS: Chronic wasting disease; Prnp; wildlife disease; population genetics; ungulates
Thursday, May 23, 2019
Prion 2019 Emerging Concepts CWD, BSE, SCRAPIE, CJD, SCIENTIFIC PROGRAM Schedule and Abstracts
see full Prion 2019 Conference Abstracts
THURSDAY, OCTOBER 04, 2018
Cervid to human prion transmission 5R01NS088604-04 Update
snip…full text;
SATURDAY, FEBRUARY 09, 2019
Experts: Yes, chronic wasting disease in deer is a public health issue — for people
FRIDAY, JULY 26, 2019
Chronic Wasting Disease in Cervids: Implications for Prion Transmission to Humans and Other Animal Species
MONDAY, FEBRUARY 25, 2019
***> MAD DOGS AND ENGLISHMEN BSE, SCRAPIE, CWD, CJD, TSE PRION A REVIEW 2019
WEDNESDAY, JULY 31, 2019
The agent of transmissible mink encephalopathy passaged in sheep is similar to BSE-L
***> cattle, pigs, sheep, cwd, tse, prion, oh my!
***> In contrast, cattle are highly susceptible to white-tailed deer CWD and mule deer CWD in experimental conditions but no natural CWD infections in cattle have been reported (Sigurdson, 2008; Hamir et al., 2006).
Sheep and cattle may be exposed to CWD via common grazing areas with affected deer but so far, appear to be poorly susceptible to mule deer CWD (Sigurdson, 2008). In contrast, cattle are highly susceptible to white-tailed deer CWD and mule deer CWD in experimental conditions but no natural CWD infections in cattle have been reported (Sigurdson, 2008; Hamir et al., 2006). It is not known how susceptible humans are to CWD but given that the prion can be present in muscle, it is likely that humans have been exposed to the agent via consumption of venison (Sigurdson, 2008). Initial experimental research suggests that human susceptibility to CWD is low and there may be a robust species barrier for CWD transmission to humans (Sigurdson, 2008), however the risk appetite for a public health threat may still find this level unacceptable.
cwd scrapie pigs oral routes
***> However, at 51 months of incubation or greater, 5 animals were positive by one or more diagnostic methods. Furthermore, positive bioassay results were obtained from all inoculated groups (oral and intracranial; market weight and end of study) suggesting that swine are potential hosts for the agent of scrapie. <***
>*** Although the current U.S. feed ban is based on keeping tissues from TSE infected cattle from contaminating animal feed, swine rations in the U.S. could contain animal derived components including materials from scrapie infected sheep and goats. These results indicating the susceptibility of pigs to sheep scrapie, coupled with the limitations of the current feed ban, indicates that a revision of the feed ban may be necessary to protect swine production and potentially human health. <***
***> Results: PrPSc was not detected by EIA and IHC in any RPLNs. All tonsils and MLNs were negative by IHC, though the MLN from one pig in the oral <6 5="" 6="" at="" by="" detected="" eia.="" examined="" group="" in="" intracranial="" least="" lymphoid="" month="" months="" of="" one="" pigs="" positive="" prpsc="" quic="" the="" tissues="" was="">6 months group, 5/6 pigs in the oral <6 4="" and="" group="" months="" oral="">6 months group. Overall, the MLN was positive in 14/19 (74%) of samples examined, the RPLN in 8/18 (44%), and the tonsil in 10/25 (40%).
***> Conclusions: This study demonstrates that PrPSc accumulates in lymphoid tissues from pigs challenged intracranially or orally with the CWD agent, and can be detected as early as 4 months after challenge. CWD-infected pigs rarely develop clinical disease and if they do, they do so after a long incubation period.
This raises the possibility that CWD-infected pigs could shed prions into their environment long before they develop clinical disease.
Furthermore, lymphoid tissues from CWD-infected pigs could present a potential source of CWD infectivity in the animal and human food chains.
Friday, December 14, 2012
DEFRA U.K. What is the risk of Chronic Wasting Disease CWD being introduced into Great Britain? A Qualitative Risk Assessment October 2012
snip.....
In the USA, under the Food and Drug Administration's BSE Feed Regulation (21 CFR 589.2000) most material (exceptions include milk, tallow, and gelatin) from deer and elk is prohibited for use in feed for ruminant animals. With regards to feed for non-ruminant animals, under FDA law, CWD positive deer may not be used for any animal feed or feed ingredients. For elk and deer considered at high risk for CWD, the FDA recommends that these animals do not enter the animal feed system. However, this recommendation is guidance and not a requirement by law.
Animals considered at high risk for CWD include:
1) animals from areas declared to be endemic for CWD and/or to be CWD eradication zones and
2) deer and elk that at some time during the 60-month period prior to slaughter were in a captive herd that contained a CWD-positive animal.
Therefore, in the USA, materials from cervids other than CWD positive animals may be used in animal feed and feed ingredients for non-ruminants.
The amount of animal PAP that is of deer and/or elk origin imported from the USA to GB can not be determined, however, as it is not specified in TRACES. It may constitute a small percentage of the 8412 kilos of non-fish origin processed animal proteins that were imported from US into GB in 2011.
Overall, therefore, it is considered there is a __greater than negligible risk___ that (nonruminant) animal feed and pet food containing deer and/or elk protein is imported into GB.
There is uncertainty associated with this estimate given the lack of data on the amount of deer and/or elk protein possibly being imported in these products.
snip.....
36% in 2007 (Almberg et al., 2011). In such areas, population declines of deer of up to 30 to 50% have been observed (Almberg et al., 2011). In areas of Colorado, the prevalence can be as high as 30% (EFSA, 2011).
The clinical signs of CWD in affected adults are weight loss and behavioural changes that can span weeks or months (Williams, 2005). In addition, signs might include excessive salivation, behavioural alterations including a fixed stare and changes in interaction with other animals in the herd, and an altered stance (Williams, 2005). These signs are indistinguishable from cervids experimentally infected with bovine spongiform encephalopathy (BSE).
Given this, if CWD was to be introduced into countries with BSE such as GB, for example, infected deer populations would need to be tested to differentiate if they were infected with CWD or BSE to minimise the risk of BSE entering the human food-chain via affected venison.
snip.....
The rate of transmission of CWD has been reported to be as high as 30% and can approach 100% among captive animals in endemic areas (Safar et al., 2008).
snip.....
In summary, in endemic areas, there is a medium probability that the soil and surrounding environment is contaminated with CWD prions and in a bioavailable form. In rural areas where CWD has not been reported and deer are present, there is a greater than negligible risk the soil is contaminated with CWD prion.
snip.....
In summary, given the volume of tourists, hunters and servicemen moving between GB and North America, the probability of at least one person travelling to/from a CWD affected area and, in doing so, contaminating their clothing, footwear and/or equipment prior to arriving in GB is greater than negligible... For deer hunters, specifically, the risk is likely to be greater given the increased contact with deer and their environment. However, there is significant uncertainty associated with these estimates.
snip.....
Therefore, it is considered that farmed and park deer may have a higher probability of exposure to CWD transferred to the environment than wild deer given the restricted habitat range and higher frequency of contact with tourists and returning GB residents.
snip.....
READ THIS VERY, VERY, CAREFULLY;
SUNDAY, SEPTEMBER 1, 2019
***> FDA Reports on VFD Compliance
TUESDAY, APRIL 18, 2017
*** EXTREME USA FDA PART 589 TSE PRION FEED LOOP HOLE STILL EXIST, AND PRICE OF POKER GOES UP ***
THURSDAY, AUGUST 08, 2019
Raccoons accumulate PrPSc after intracranial inoculation with the agents of chronic wasting disease (CWD) or transmissible mink encephalopathy (TME) but not atypical scrapie
SUNDAY, SEPTEMBER 08, 2019
Wisconsin Laboratory Testing Options for Prion Diseases, Wisconsin Neurologists, Clinical Laboratory Directors, and Infection Preventionists, Please Distribute Widely
Preparing for the Storm
the British disease...NOT, the UKBSEnvCJD only theory was/is bogus $$$
*** USA sporadic CJD MAD COW DISEASE HAS HUGE PROBLEM Video
*** sporadic CJD linked to mad cow disease
*** you can see video here and interview with Jeff's Mom, and scientist telling you to test everything and potential risk factors for humans ***
MONDAY, JUNE 24, 2019
APHIS, FSIS, USDA, FDA, Transmissible Spongiform Encephalopathy TSE, BSE, CWD, Scrapie, Camel TSE Prion Disease, CJD Humans
WEDNESDAY, JULY 31, 2019
The agent of transmissible mink encephalopathy passaged in sheep is similar to BSE-L
TUESDAY, JULY 30, 2019
Guidelines for reporting surveillance data on Transmissible Spongiform Encephalopathies (TSE) in the EU within the framework of Regulation (EC) No 999/2001 APPROVED: 9 July 2019
THURSDAY, FEBRUARY 28, 2019
BSE infectivity survives burial for five years with only limited spread
SUNDAY, APRIL 14, 2019
Estimation of prion infectivity in tissues of cattle infected with atypical BSE by real time-quaking induced conversion assay
MONDAY, MAY 20, 2019
Tracking and clarifying differential traits of classical- and atypical L-type bovine spongiform encephalopathy prions after transmission from cattle to cynomolgus monkeys
WEDNESDAY, APRIL 24, 2019
USDA Announces Atypical Bovine Spongiform Encephalopathy Detection Aug 29, 2018 A Review of Science 2019
O.05: Transmission of prions to primates after extended silent incubation periods: Implications for BSE and scrapie risk assessment in human populations
Emmanuel Comoy, Jacqueline Mikol, Valerie Durand, Sophie Luccantoni, Evelyne Correia, Nathalie Lescoutra, Capucine Dehen, and Jean-Philippe Deslys Atomic Energy Commission; Fontenay-aux-Roses, France
Prion diseases (PD) are the unique neurodegenerative proteinopathies reputed to be transmissible under field conditions since decades. The transmission of Bovine Spongiform Encephalopathy (BSE) to humans evidenced that an animal PD might be zoonotic under appropriate conditions. Contrarily, in the absence of obvious (epidemiological or experimental) elements supporting a transmission or genetic predispositions, PD, like the other proteinopathies, are reputed to occur spontaneously (atpical animal prion strains, sporadic CJD summing 80% of human prion cases).
Non-human primate models provided the first evidences supporting the transmissibiity of human prion strains and the zoonotic potential of BSE. Among them, cynomolgus macaques brought major information for BSE risk assessment for human health (Chen, 2014), according to their phylogenetic proximity to humans and extended lifetime. We used this model to assess the zoonotic potential of other animal PD from bovine, ovine and cervid origins even after very long silent incubation periods.
*** We recently observed the direct transmission of a natural classical scrapie isolate to macaque after a 10-year silent incubation period,
***with features similar to some reported for human cases of sporadic CJD, albeit requiring fourfold long incubation than BSE. Scrapie, as recently evoked in humanized mice (Cassard, 2014),
***is the third potentially zoonotic PD (with BSE and L-type BSE),
***thus questioning the origin of human sporadic cases.
We will present an updated panorama of our different transmission studies and discuss the implications of such extended incubation periods on risk assessment of animal PD for human health.
===============
***thus questioning the origin of human sporadic cases***
===============
***our findings suggest that possible transmission risk of H-type BSE to sheep and human. Bioassay will be required to determine whether the PMCA products are infectious to these animals.
==============
***Transmission data also revealed that several scrapie prions propagate in HuPrP-Tg mice with efficiency comparable to that of cattle BSE. While the efficiency of transmission at primary passage was low, subsequent passages resulted in a highly virulent prion disease in both Met129 and Val129 mice.
***Transmission of the different scrapie isolates in these mice leads to the emergence of prion strain phenotypes that showed similar characteristics to those displayed by MM1 or VV2 sCJD prion.
***These results demonstrate that scrapie prions have a zoonotic potential and raise new questions about the possible link between animal and human prions.
PRION 2016 TOKYO
Saturday, April 23, 2016
SCRAPIE WS-01: Prion diseases in animals and zoonotic potential 2016
Prion. 10:S15-S21. 2016 ISSN: 1933-6896 printl 1933-690X online
Taylor & Francis
Prion 2016 Animal Prion Disease Workshop Abstracts
WS-01: Prion diseases in animals and zoonotic potential
Juan Maria Torres a, Olivier Andreoletti b, J uan-Carlos Espinosa a. Vincent Beringue c. Patricia Aguilar a,
Natalia Fernandez-Borges a. and Alba Marin-Moreno a
"Centro de Investigacion en Sanidad Animal ( CISA-INIA ). Valdeolmos, Madrid. Spain; b UMR INRA -ENVT 1225 Interactions Holes Agents Pathogenes. ENVT. Toulouse. France: "UR892. Virologie lmmunologie MolécuIaires, Jouy-en-Josas. France
Dietary exposure to bovine spongiform encephalopathy (BSE) contaminated bovine tissues is considered as the origin of variant Creutzfeldt Jakob (vCJD) disease in human. To date, BSE agent is the only recognized zoonotic prion... Despite the variety of Transmissible Spongiform Encephalopathy (TSE) agents that have been circulating for centuries in farmed ruminants there is no apparent epidemiological link between exposure to ruminant products and the occurrence of other form of TSE in human like sporadic Creutzfeldt Jakob Disease (sCJD). However, the zoonotic potential of the diversity of circulating TSE agents has never been systematically assessed. The major issue in experimental assessment of TSEs zoonotic potential lies in the modeling of the ‘species barrier‘, the biological phenomenon that limits TSE agents’ propagation from a species to another. In the last decade, mice genetically engineered to express normal forms of the human prion protein has proved essential in studying human prions pathogenesis and modeling the capacity of TSEs to cross the human species barrier.
To assess the zoonotic potential of prions circulating in farmed ruminants, we study their transmission ability in transgenic mice expressing human PrPC (HuPrP-Tg). Two lines of mice expressing different forms of the human PrPC (129Met or 129Val) are used to determine the role of the Met129Val dimorphism in susceptibility/resistance to the different agents.
These transmission experiments confirm the ability of BSE prions to propagate in 129M- HuPrP-Tg mice and demonstrate that Met129 homozygotes may be susceptible to BSE in sheep or goat to a greater degree than the BSE agent in cattle and that these agents can convey molecular properties and neuropathological indistinguishable from vCJD. However homozygous 129V mice are resistant to all tested BSE derived prions independently of the originating species suggesting a higher transmission barrier for 129V-PrP variant.
Transmission data also revealed that several scrapie prions propagate in HuPrP-Tg mice with efficiency comparable to that of cattle BSE. While the efficiency of transmission at primary passage was low, subsequent passages resulted in a highly virulent prion disease in both Met129 and Val129 mice.
Transmission of the different scrapie isolates in these mice leads to the emergence of prion strain phenotypes that showed similar characteristics to those displayed by MM1 or VV2 sCJD prion.
These results demonstrate that scrapie prions have a zoonotic potential and raise new questions about the possible link between animal and human prions.
***> why do we not want to do TSE transmission studies on chimpanzees $
5. A positive result from a chimpanzee challenged severly would likely create alarm in some circles even if the result could not be interpreted for man.
***> I have a view that all these agents could be transmitted provided a large enough dose by appropriate routes was given and the animals kept long enough.
***> Until the mechanisms of the species barrier are more clearly understood it might be best to retain that hypothesis.
snip...
R. BRADLEY
Title: Transmission of scrapie prions to primate after an extended silent incubation period)
*** In complement to the recent demonstration that humanized mice are susceptible to scrapie, we report here the first observation of direct transmission of a natural classical scrapie isolate to a macaque after a 10-year incubation period. Neuropathologic examination revealed all of the features of a prion disease: spongiform change, neuronal loss, and accumulation of PrPres throughout the CNS.
*** This observation strengthens the questioning of the harmlessness of scrapie to humans, at a time when protective measures for human and animal health are being dismantled and reduced as c-BSE is considered controlled and being eradicated.
*** Our results underscore the importance of precautionary and protective measures and the necessity for long-term experimental transmission studies to assess the zoonotic potential of other animal prion strains.
***> Moreover, sporadic disease has never been observed in breeding colonies or primate research laboratories, most notably among hundreds of animals over several decades of study at the National Institutes of Health25, and in nearly twenty older animals continuously housed in our own facility. <***
Transmission of scrapie prions to primate after an extended silent incubation period
Emmanuel E. Comoy, Jacqueline Mikol, Sophie Luccantoni-Freire, Evelyne Correia, Nathalie Lescoutra-Etchegaray, Valérie Durand, Capucine Dehen, Olivier Andreoletti, Cristina Casalone, Juergen A. Richt, Justin J. Greenlee, Thierry Baron, Sylvie L. Benestad, Paul Brown & Jean-Philippe Deslys Scientific Reports volume 5, Article number: 11573 (2015) | Download Citation
Abstract
Classical bovine spongiform encephalopathy (c-BSE) is the only animal prion disease reputed to be zoonotic, causing variant Creutzfeldt-Jakob disease (vCJD) in humans and having guided protective measures for animal and human health against animal prion diseases. Recently, partial transmissions to humanized mice showed that the zoonotic potential of scrapie might be similar to c-BSE. We here report the direct transmission of a natural classical scrapie isolate to cynomolgus macaque, a highly relevant model for human prion diseases, after a 10-year silent incubation period, with features similar to those reported for human cases of sporadic CJD. Scrapie is thus actually transmissible to primates with incubation periods compatible with their life expectancy, although fourfold longer than BSE. Long-term experimental transmission studies are necessary to better assess the zoonotic potential of other prion diseases with high prevalence, notably Chronic Wasting Disease of deer and elk and atypical/Nor98 scrapie.
SNIP...
Discussion We describe the transmission of spongiform encephalopathy in a non-human primate inoculated 10 years earlier with a strain of sheep c-scrapie. Because of this extended incubation period in a facility in which other prion diseases are under study, we are obliged to consider two alternative possibilities that might explain its occurrence. We first considered the possibility of a sporadic origin (like CJD in humans). Such an event is extremely improbable because the inoculated animal was 14 years old when the clinical signs appeared, i.e. about 40% through the expected natural lifetime of this species, compared to a peak age incidence of 60–65 years in human sporadic CJD, or about 80% through their expected lifetimes. Moreover, sporadic disease has never been observed in breeding colonies or primate research laboratories, most notably among hundreds of animals over several decades of study at the National Institutes of Health25, and in nearly twenty older animals continuously housed in our own facility.
The second possibility is a laboratory cross-contamination. Three facts make this possibility equally unlikely. First, handling of specimens in our laboratory is performed with fastidious attention to the avoidance of any such cross-contamination. Second, no laboratory cross-contamination has ever been documented in other primate laboratories, including the NIH, even between infected and uninfected animals housed in the same or adjacent cages with daily intimate contact (P. Brown, personal communication). Third, the cerebral lesion profile is different from all the other prion diseases we have studied in this model19, with a correlation between cerebellar lesions (massive spongiform change of Purkinje cells, intense PrPres staining and reactive gliosis26) and ataxia. The iron deposits present in the globus pallidus are a non specific finding that have been reported previously in neurodegenerative diseases and aging27. Conversely, the thalamic lesion was reminiscent of a metabolic disease due to thiamine deficiency28 but blood thiamine levels were within normal limits (data not shown). The preferential distribution of spongiform change in cortex associated with a limited distribution in the brainstem is reminiscent of the lesion profile in MM2c and VV1 sCJD patients29, but interspecies comparison of lesion profiles should be interpreted with caution. It is of note that the same classical scrapie isolate induced TSE in C57Bl/6 mice with similar incubation periods and lesional profiles as a sample derived from a MM1 sCJD patient30.
We are therefore confident that the illness in this cynomolgus macaque represents a true transmission of a sheep c-scrapie isolate directly to an old-world monkey, which taxonomically resides in the primate subdivision (parvorder of catarrhini) that includes humans. With an homology of its PrP protein with humans of 96.4%31, cynomolgus macaque constitutes a highly relevant model for assessing zoonotic risk of prion diseases. Since our initial aim was to show the absence of transmission of scrapie to macaques in the worst-case scenario, we obtained materials from a flock of naturally-infected sheep, affecting animals with different genotypes32. This c-scrapie isolate exhibited complete transmission in ARQ/ARQ sheep (332 ± 56 days) and Tg338 transgenic mice expressing ovine VRQ/VRQ prion protein (220 ± 5 days) (O. Andreoletti, personal communication). From the standpoint of zoonotic risk, it is important to note that sheep with c-scrapie (including the isolate used in our study) have demonstrable infectivity throughout their lymphoreticular system early in the incubation period of the disease (3 months-old for all the lymphoid organs, and as early as 2 months-old in gut-associated lymph nodes)33. In addition, scrapie infectivity has been identified in blood34, milk35 and skeletal muscle36 from asymptomatic but scrapie infected small ruminants which implies a potential dietary exposure for consumers.
Two earlier studies have reported the occurrence of clinical TSE in cynomolgus macaques after exposures to scrapie isolates. In the first study, the “Compton” scrapie isolate (derived from an English sheep) and serially propagated for 9 passages in goats did not transmit TSE in cynomolgus macaque, rhesus macaque or chimpanzee within 7 years following intracerebral challenge1; conversely, after 8 supplementary passages in conventional mice, this “Compton” isolate induced TSE in a cynomolgus macaque 5 years after intracerebral challenge, but rhesus macaques and chimpanzee remained asymptomatic 8.5 years post-exposure8. However, multiple successive passages that are classically used to select laboratory-adapted prion strains can significantly modify the initial properties of a scrapie isolate, thus questioning the relevance of zoonotic potential for the initial sheep-derived isolate. The same isolate had also induced disease into squirrel monkeys (new-world monkey)9. A second historical observation reported that a cynomolgus macaque developed TSE 6 years post-inoculation with brain homogenate from a scrapie-infected Suffolk ewe (derived from USA), whereas a rhesus macaque and a chimpanzee exposed to the same inoculum remained healthy 9 years post-exposure1. This inoculum also induced TSE in squirrel monkeys after 4 passages in mice. Other scrapie transmission attempts in macaque failed but had more shorter periods of observation in comparison to the current study. Further, it is possible that there are differences in the zoonotic potential of different scrapie strains.
The most striking observation in our study is the extended incubation period of scrapie in the macaque model, which has several implications. Firstly, our observations constitute experimental evidence in favor of the zoonotic potential of c-scrapie, at least for this isolate that has been extensively studied32,33,34,35,36. The cross-species zoonotic ability of this isolate should be confirmed by performing duplicate intracerebral exposures and assessing the transmissibility by the oral route (a successful transmission of prion strains through the intracerebral route may not necessarily indicate the potential for oral transmission37). However, such confirmatory experiments may require more than one decade, which is hardly compatible with current general management and support of scientific projects; thus this study should be rather considered as a case report.
Secondly, transmission of c-BSE to primates occurred within 8 years post exposure for the lowest doses able to transmit the disease (the survival period after inoculation is inversely proportional to the initial amount of infectious inoculum). The occurrence of scrapie 10 years after exposure to a high dose (25 mg) of scrapie-infected sheep brain suggests that the macaque has a higher species barrier for sheep c-scrapie than c-BSE, although it is notable that previous studies based on in vitro conversion of PrP suggested that BSE and scrapie prions would have a similar conversion potential for human PrP38.
Thirdly, prion diseases typically have longer incubation periods after oral exposure than after intracerebral inoculations: since humans can develop Kuru 47 years after oral exposure39, an incubation time of several decades after oral exposure to scrapie would therefore be expected, leading the disease to occur in older adults, i.e. the peak age for cases considered to be sporadic disease, and making a distinction between scrapie-associated and truly sporadic disease extremely difficult to appreciate.
Fourthly, epidemiologic evidence is necessary to confirm the zoonotic potential of an animal disease suggested by experimental studies. A relatively short incubation period and a peculiar epidemiological situation (e.g., all the first vCJD cases occurring in the country with the most important ongoing c-BSE epizootic) led to a high degree of suspicion that c-BSE was the cause of vCJD. Sporadic CJD are considered spontaneous diseases with an almost stable and constant worldwide prevalence (0.5–2 cases per million inhabitants per year), and previous epidemiological studies were unable to draw a link between sCJD and classical scrapie6,7,40,41, even though external causes were hypothesized to explain the occurrence of some sCJD clusters42,43,44. However, extended incubation periods exceeding several decades would impair the predictive values of epidemiological surveillance for prion diseases, already weakened by a limited prevalence of prion diseases and the multiplicity of isolates gathered under the phenotypes of “scrapie” and “sporadic CJD”.
Fifthly, considering this 10 year-long incubation period, together with both laboratory and epidemiological evidence of decade or longer intervals between infection and clinical onset of disease, no premature conclusions should be drawn from negative transmission studies in cynomolgus macaques with less than a decade of observation, as in the aforementioned historical transmission studies of scrapie to primates1,8,9. Our observations and those of others45,46 to date are unable to provide definitive evidence regarding the zoonotic potential of CWD, atypical/Nor98 scrapie or H-type BSE. The extended incubation period of the scrapie-affected macaque in the current study also underscores the limitations of rodent models expressing human PrP for assessing the zoonotic potential of some prion diseases since their lifespan remains limited to approximately two years21,47,48. This point is illustrated by the fact that the recently reported transmission of scrapie to humanized mice was not associated with clinical signs for up to 750 days and occurred in an extreme minority of mice with only a marginal increase in attack rate upon second passage13. The low attack rate in these studies is certainly linked to the limited lifespan of mice compared to the very long periods of observation necessary to demonstrate the development of scrapie. Alternatively, one could estimate that a successful second passage is the result of strain adaptation to the species barrier, thus poorly relevant of the real zoonotic potential of the original scrapie isolate of sheep origin49. The development of scrapie in this primate after an incubation period compatible with its lifespan complements the study conducted in transgenic (humanized) mice; taken together these studies suggest that some isolates of sheep scrapie can promote misfolding of the human prion protein and that scrapie can develop within the lifespan of some primate species.
In addition to previous studies on scrapie transmission to primate1,8,9 and the recently published study on transgenic humanized mice13, our results constitute new evidence for recommending that the potential risk of scrapie for human health should not be dismissed. Indeed, human PrP transgenic mice and primates are the most relevant models for investigating the human transmission barrier. To what extent such models are informative for measuring the zoonotic potential of an animal TSE under field exposure conditions is unknown. During the past decades, many protective measures have been successfully implemented to protect cattle from the spread of c-BSE, and some of these measures have been extended to sheep and goats to protect from scrapie according to the principle of precaution. Since cases of c-BSE have greatly reduced in number, those protective measures are currently being challenged and relaxed in the absence of other known zoonotic animal prion disease. We recommend that risk managers should be aware of the long term potential risk to human health of at least certain scrapie isolates, notably for lymphotropic strains like the classical scrapie strain used in the current study. Relatively high amounts of infectivity in peripheral lymphoid organs in animals infected with these strains could lead to contamination of food products produced for human consumption. Efforts should also be maintained to further assess the zoonotic potential of other animal prion strains in long-term studies, notably lymphotropic strains with high prevalence like CWD, which is spreading across North America, and atypical/Nor98 scrapie (Nor98)50 that was first detected in the past two decades and now represents approximately half of all reported cases of prion diseases in small ruminants worldwide, including territories previously considered as scrapie free... Even if the prevailing view is that sporadic CJD is due to the spontaneous formation of CJD prions, it remains possible that its apparent sporadic nature may, at least in part, result from our limited capacity to identify an environmental origin.
THURSDAY, SEPTEMBER 26, 2019
Veterinary Biologics Guideline 3.32E: Guideline for minimising the risk of introducing transmissible spongiform encephalopathy prions and other infectious agents through veterinary biologics
SATURDAY, SEPTEMBER 21, 2019
National Variability in Prion Disease–Related Safety Policies for Neurologic Procedures
Friday, September 27, 2019
Prion disease and recommended procedures for flexible endoscope reprocessing – a review of policies worldwide and proposal for a simplified approach
Singeltary 2003 submission to GUT warning of the same thing...
THURSDAY, SEPTEMBER 26, 2019
USDA Scientific Integrity Policy Departmental Regulation 1074-001 Breached
What you need to know about archery hunting in CWD areas
Wondering exactly what’s expected of bowhunters in CWD surveillance areas? Check out this webpage, which walks hunters through each step and provides information on restrictions, locations of sampling stations and dumpsters, shows photos of what you can expect at a self-service sampling station, and much more!
|
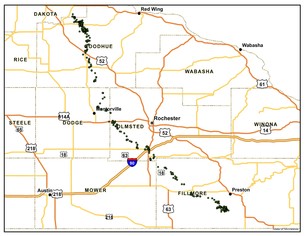 Deer movement study update
After collaring 64 additional deer with GPS collars in February, we watched 56 yearlings as they went through their spring dispersal period from April through July, when deer typically make their longest journeys. About half of them made what appear to be one-way, long-distance movements from their birthplaces, but we may see some of them come back as fall settles in.
As for deer collared last year, several deer appear to be making seasonal movements between multiple home ranges, which is not expected of deer in this area and is a behavior we'll be watching closely.
Follow updates on the southeast deer movement study webpage, where you can check out the newest deer movement maps.
The above map shows the movement of a female deer, Ear Tag 111, from March 2018 through February 2019. Each dot represents her location as it was transmitted by a GPS collar every 1-2 hours; she traveled 77 miles from Fillmore County to Goodhue County the summer after she was born.
|
 CWD resources for 2019: new videos, interactive maps
Check out our new videos for the 2019 season! Added for this year: how to provide a sample at a self-service sampling station; the top things hunters need to know about CWD; and important information about carcass movement restrictions. You can find all of our videos — including information on how to quarter a deer, cape a trophy deer or remove a deer’s lymph nodes for sampling — on the CWD videos page.
We’ve also added interactive maps to our webpages to make it easier to zoom in on the information you need, like sampling stations or carcass disposal stations.
|
CWD testing requirements: no matter the hunt, know your zone
No matter what hunting season or special hunt you’re participating in, all hunters need to remember that certain restrictions are in place in areas that CWD was discovered in wild or captive deer. This includes youth season, early antlerless season and all special hunts. (Failure to submit a sample for special hunts may disqualify the hunter from eligibility in future special hunts and result in a monetary fine.)
Pay attention to the rules in these areas (southeast, north central and central Minnesota), which include mandatory sampling and carcass movement restrictions. Find more information at mndnr.gov/cwd.
Help with CWD efforts by adopting a carcass disposal location
Looking for a way to help out with CWD management efforts? The Adopt-A-Dumpster program allows individuals and groups to sponsor sites to help hunters properly dispose of deer remains and comply with deer carcass movement restrictions.
You can help by:
- Monitoring dumpsters (keep the area free of litter; reposition cover to keep out rain and snow).
- Donating funds to cover all or partial costs of a dumpster location.
To get involved or find out more details, please contact Bryan Lueth at bryan.lueth@state.mn.us or 651-259-5190.
THURSDAY, MAY 09, 2019
Minnesota Seven deer test positive for CWD at Crow Wing County deer farm
***> The USDA is providing indemnity to the owner for the animals as part of its overall disease control effort.
off the taxpayers back $$$
'indemnity' nothing but an entitlement program...imo.
CWD-positive deer found in Crow Wing County
The DNR has confirmed chronic wasting disease in a wild deer in Crow Wing County. This test result marks the first time in Minnesota the always-fatal neurological disease has been found in a wild deer outside of the southeastern part of the state. The DNR is targeting a localized area to remove infected deer. It is offering landowner shooting permits and working with willing landowners to allow the U.S. Department of Agriculture to remove additional deer on their properties.
The Crow Wing County deer, an adult female, was found Jan. 23 on the northwest side of Upper Mission Lake, northeast of the town of Merrifield. A conservation officer responded to a report of a deceased deer in the area. Test results confirmed the deer as positive for CWD on Feb. 14. The necropsy report is available on the north central Minnesota CWD management page.
FRIDAY, FEBRUARY 15, 2019
Minnesota New CWD-positive deer in Crow Wing County and southeastern Minnesota require additional disease monitoring and management
THURSDAY, DECEMBER 06, 2018
Minnesota Wild deer identified as presumptive positive for CWD outside of disease management zone first in Houston County
FRIDAY, NOVEMBER 09, 2018
Minnesota CWD TSE Prion detected four harvested samples from farmed deer quarantined farm Crow Wing County
SATURDAY, APRIL 21, 2018
MINNESOTA STATE AUDITORS Board of Animal Health has failed to enforce some laws relating to deer and elk farms A CWD TSE PRION GLOBAL UPDATE
THURSDAY, APRIL 12, 2018
Minnesota DNR's 10-year CWD TSE Prion deer plan?
MONDAY, AUGUST 28, 2017
Minnesota CWD tests mandatory for deer harvested in central, north-central and southeast
SUNDAY, AUGUST 20, 2017
Minnesota Fearing spread of CWD, agency pushing animal health board to suspend farmer's license
FRIDAY, JANUARY 20, 2017
Minnesota Chronic Wasting Disease investigation traces exposure to Meeker County farm
WEDNESDAY, APRIL 17, 2019
Minnesota Board of Animal Health CWD positive Crow Wing County deer farm depopulated
Sent: Sun, Apr 14, 2019 11:28 am
Subject: Chronic Wasting Disease TSE Prion Strains everything in Texas is bigger, better, and badder
One day in late February, in their laboratory in Fort Collins, Colorado, Wagner and Zabel compared the prions from the brains of CWD-infected deer in Texas with those of elk in Colorado. They want to know if the proteins were all mangled in the same way, or not. “If they are different, this would suggest that we have different strain properties, which is evidence as we're building our case that we might have multiple strains of CWD circulating in the U.S.,” says Wagner.
Step one is to see if they’re equally easy to destroy using a chemical called guanidine. The shape of a prion dictates everything, including the way it interacts with an animal’s cells and the ease with which chemicals can unfold it.
“Moment of truth,” said Wagner, as she and Zabel huddled around a computer, waiting for results to come through. When they did, Zabel was surprised.
“Wow,” he said. “Unlike anything we've seen before.”
The prions from the Texas deer were a lot harder to destroy than the ones from the Colorado elk. In fact, the guanidine barely damaged them at all. “We’ve never seen that before in any prion strain, which means that it has a completely different structure than we've ever seen before,” says Zabel. And that suggests that it might be a very different kind of chronic wasting disease. The researchers ran the same test on another Texas deer, with the same results.
snip...see full text;
SUNDAY, APRIL 14, 2019
Chronic Wasting Disease TSE Prion Strains everything in Texas is bigger, better, and badder
77. Assessing chronic wasting disease strain differences in free-ranging cervids across the United States
Kaitlyn M. Wagnera, Caitlin Ott-Connb, Kelly Strakab, Bob Dittmarc, Jasmine Battend, Robyn Piercea, Mercedes Hennessya, Elizabeth Gordona, Brett Israela, Jenn Ballarde and Mark D Zabela
aPrion Research Center at Colorado State University; bMichigan Department of Natural Resources; cTexas Parks and Wildlife Department; dMissouri Department of Conservation, 5. Arkansas Game and Fish Commission
CONTACT Kaitlyn M. Wagner miedkait@rams.colostate.edu
ABSTRACT
Background/Introduction: Chronic wasting disease (CWD) is an invariably fatal prion disease affecting captive and free-ranging cervids, including white-tailed deer, mule deer, moose, elk, and reindeer. Since the initial description of the disease in the 1960’s, CWD has spread to 23 states, 3 Canadian Provinces, South Korea, Norway and, most recently, Finland. While some outbreaks of CWD were caused by transport of infected animals from endemic regions, the origin of CWD in other epizootics is unclear and has not been characterized. Previous studies have shown that there are two distinct strains of CWD. However, the continuous spread and the unclear origin of several outbreaks warrant continued surveillance and further characterization of strain diversity.
Materials and Methods: To address these knowledge gaps, we used biochemical tests to assess strain differences between CWD outbreaks in Michigan, Texas, Missouri, and Colorado, USA. Brain or lymph node samples were homogenized and digested in 50 µg/mL proteinase K (PK). These samples were then run on a Western blot to assess glycoform ratio and electrophoretic mobility. Texas samples were digested in 100 µg/mL PK. To assess conformational stability, brain or lymph node homogenates were incubated in increasing concentrations of guanidine hydrochloride from 0 M to 4 M in 0.5 M increments. Samples were then precipitated in methanol overnight, washed and PK digested in 50 µg/mL PK before slot blotting.
Results: Our results have found significant differences in glycoform ratio between CWD from Michigan and Colorado, but no differences were observed in conformational stability assays. Interestingly, when testing our CWD isolates from Texas to analyse electrophoretic mobility and glycoform ratio, we found that these samples did not exhibit the characteristic band shift when treated with PK, but PK resistant material remained. Additionally, results from our conformational stability assay demonstrate a unique profile of these Texas isolates. Testing of samples from Missouri is currently underway.
Conclusions: Thus far, our data indicate that there are strain differences between CWD circulating in Michigan and CWD in Colorado and provide important insight into CWD strain differences between two non-contiguous outbreaks. We have also identified a unique strain of CWD in Texas with biochemical strain properties not seen in any of our other CWD isolates. These results highlight the importance of continued surveillance to better understand this devastating disease. These results have important implications for CWD emergence, evolution and our understanding of prion strain heterogeneity on the landscape.
TEXAS CWD TSE PRION STRAIN UNLIKE ANYTHING EVER SEEN
“Wow,” he said. “Unlike anything we've seen before.”
The prions from the Texas deer were a lot harder to destroy than the ones from the Colorado elk. In fact, the guanidine barely damaged them at all. “We’ve never seen that before in any prion strain, which means that it has a completely different structure than we've ever seen before,” says Zabel. And that suggests that it might be a very different kind of chronic wasting disease. The researchers ran the same test on another Texas deer, with the same results.
snip...
“Wow,” he said. “Unlike anything we've seen before.”
The prions from the Texas deer were a lot harder to destroy than the ones from the Colorado elk. In fact, the guanidine barely damaged them at all. “We’ve never seen that before in any prion strain, which means that it has a completely different structure than we've ever seen before,” says Zabel. And that suggests that it might be a very different kind of chronic wasting disease. The researchers ran the same test on another Texas deer, with the same results.
Now, these are only the preliminary results from a few animals. Wagner and Zabel have a lot more experiments to do. But if future tests come to the same conclusion, it would support their hypothesis that there are multiple strains of chronic wasting disease out there, all with different origins. That, in turn, could mean that this disease will become even trickier to manage than it already is.
And, Zabel adds, there’s something else. “If it's still evolving, it may still evolve into a form that could potentially, eventually affect humans,” he says.
Zabel is not the only one worried about that possibility.
OSTERHOLM, THE EPIDEMIOLOGIST from Minnesota, is also concerned. He directs the Center for Infectious Disease Research and Policy at the University of Minnesota, and is serving a one-year stint as a “Science Envoy for Health Security” with the U.S. State Department. In February, he told Minnesota lawmakers that when it comes to chronic wasting disease, we are playing with fire. “You are going to hear from people that this is not going to be a problem other than a game farm issue. You're going to hear from people that it's not going to transmit to people, and I hope they're right, but I wouldn't bet on it,” he said. “And if we lose this one and haven’t done all we can do, we will pay a price.”
If that wasn’t warning enough, he added: “Just remember what happened in England.”
THURSDAY, SEPTEMBER 05, 2019
Unique Profile of The Texas CWD TSE Prion isolates, the TSE Prion CWD, Scrapie, BSE in Livestock, and CJD in Humans
TUESDAY, NOVEMBER 20, 2018
WISCONSIN Captive CWD TSE Prion Lotto Entitlement Program Pays Out Again Indemnity From Taxpayers $330,000 To Farmers So Far This Year
Sunday, January 17, 2016
*** Wisconsin Captive CWD Lotto Pays Out Again indemnity payment of $298,770 for 228 white-tailed deer killed on farm ***
SUNDAY, DECEMBER 02, 2018
CWD TSE PRION, REGULATORY LEGISLATION, PAY TO PLAY, and The SPREAD of Chronic Wasting Disease
SUNDAY, MAY 14, 2017
85th Legislative Session 2017 AND THE TEXAS TWO STEP Chronic Wasting Disease CWD TSE Prion, and paying to play, a lesson on how political and corporate science helps spread a deadly disease
MONDAY, OCTOBER 07, 2019
Chronic Wasting Disease (CWD) and Government Response Congressional Research Service May 17, 2019
WEDNESDAY, OCTOBER 02, 2019
Chronic Wasting Disease In Cervids: Prevalence, Impact And Management Strategies
TUESDAY, SEPTEMBER 17, 2019
Michigan House Bill 4687 State Legislators Turn To Draft Dodger Ted Nugent To Make Scientific Decisions over DNR on CWD TSE Prion
Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2019
2009
On behalf of the Scientific Committee, I am pleased to inform you that your abstract
'Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009'
WAS accepted for inclusion in the INTERNATIONAL SCIENTIFIC EXCHANGE (ISE) section of the 14th International Congress on Infectious Diseases. Accordingly, your abstract will be included in the "Intl. Scientific Exchange abstract CD-rom" of the Congress which will be distributed to all participants.
Abstracts accepted for INTERNATIONAL SCIENTIFIC EXCHANGE are NOT PRESENTED in the oral OR poster sessions.
Your abstract below was accepted for: INTERNATIONAL SCIENTIFIC EXCHANGE
#0670: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Author: T. Singeltary; Bacliff, TX/US
Topic: Emerging Infectious Diseases Preferred type of presentation: International Scientific Exchange
This abstract has been ACCEPTED.
#0670: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Authors: T. Singeltary; Bacliff, TX/US
Title: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Body: Background
An update on atypical BSE and other TSE in North America. Please remember, the typical U.K. c-BSE, the atypical l-BSE (BASE), and h-BSE have all been documented in North America, along with the typical scrapie's, and atypical Nor-98 Scrapie, and to date, 2 different strains of CWD, and also TME. All these TSE in different species have been rendered and fed to food producing animals for humans and animals in North America (TSE in cats and dogs ?), and that the trading of these TSEs via animals and products via the USA and Canada has been immense over the years, decades.
Methods
12 years independent research of available data
Results
I propose that the current diagnostic criteria for human TSEs only enhances and helps the spreading of human TSE from the continued belief of the UKBSEnvCJD only theory in 2009. With all the science to date refuting it, to continue to validate this old myth, will only spread this TSE agent through a multitude of potential routes and sources i.e. consumption, medical i.e., surgical, blood, dental, endoscopy, optical, nutritional supplements, cosmetics etc.
Conclusion
I would like to submit a review of past CJD surveillance in the USA, and the urgent need to make all human TSE in the USA a reportable disease, in every state, of every age group, and to make this mandatory immediately without further delay. The ramifications of not doing so will only allow this agent to spread further in the medical, dental, surgical arena's. Restricting the reporting of CJD and or any human TSE is NOT scientific. Iatrogenic CJD knows NO age group, TSE knows no boundaries.
I propose as with Aguzzi, Asante, Collinge, Caughey, Deslys, Dormont, Gibbs, Gajdusek, Ironside, Manuelidis, Marsh, et al and many more, that the world of TSE Transmissible Spongiform Encephalopathy is far from an exact science, but there is enough proven science to date that this myth should be put to rest once and for all, and that we move forward with a new classification for human and animal TSE that would properly identify the infected species, the source species, and then the route.
Keywords: Transmissible Spongiform Encephalopathy Creutzfeldt Jakob Disease Prion
page 114 ;
http://ww2.isid.org/Downloads/14th_ICID_ISE_Abstracts.pdf
http://www.isid.org/14th_icid/
http://www.isid.org/publications/ICID_Archive.shtml
http://ww2.isid.org/Downloads/IMED2009_AbstrAuth.pdf
***however in 1 C-type challenged animal, Prion 2015 Poster Abstracts
S67 PrPsc was not detected using rapid tests for BSE.
***Subsequent testing resulted in the detection of pathologic lesion in unusual brain location and PrPsc detection by PMCA only.
*** IBNC Tauopathy or TSE Prion disease, it appears, no one is sure ***
Posted by Terry S. Singeltary Sr. on 03 Jul 2015 at 16:53 GMT
P.9.21
Molecular characterization of BSE in Canada
Jianmin Yang 1 , Sandor Dudas 2 , Catherine Graham 2 , Markus Czub 3 , Tim McAllister 1 , Stefanie Czub 1 1 Agriculture and Agri-Food Canada Research Centre, Canada; 2 National and OIE BSE Reference Laboratory, Canada; 3 University of Calgary, Canada
Background: Three BSE types (classical and two atypical) have been identified on the basis of molecular characteristics of the misfolded protein associated with the disease. To date, each of these three types have been detected in Canadian cattle. Objectives: This study was conducted to further characterize the 16 Canadian BSE cases based on the biochemical properties of there associated PrPres.
Methods: Immuno-reactivity, molecular weight, glycoform profiles and relative proteinase K sensitivity of the PrPres from each of the 16 confirmed Canadian BSE cases was determined using modified Western blot analysis.
Results: Fourteen of the 16 Canadian BSE cases were C type, 1 was H type and 1 was L type. The Canadian H and L-type BSE cases exhibited size shifts and changes in glycosylation similar to other atypical BSE cases. PK digestion under mild and stringent conditions revealed a reduced protease resistance of the atypical cases compared to the C-type cases. N terminal-specific antibodies bound to PrPres from H type but not from C or L type. The C-terminal-specific antibodies resulted in a shift in the glycoform profile and detected a fourth band in the Canadian H-type BSE.
Discussion: The C, L and H type BSE cases in Canada exhibit molecular characteristics similar to those described for classical and atypical BSE cases from Europe and Japan. This supports the theory that the importation of BSE contaminated feedstuff is the source of C-type BSE in Canada. It also suggests a similar cause or source for atypical BSE in these countries.
Discussion: The C, L and H type BSE cases in Canada exhibit molecular characteristics similar to those described for classical and atypical BSE cases from Europe and Japan.
*** This supports the theory that the importation of BSE contaminated feedstuff is the source of C-type BSE in Canada.
*** It also suggests a similar cause or source for atypical BSE in these countries. ***
see page 176 of 201 pages...tss
*** Singeltary reply ; Molecular, Biochemical and Genetic Characteristics of BSE in Canada Singeltary reply;
Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2019
SUNDAY, SEPTEMBER 1, 2019
FDA Reports on VFD Compliance
SUNDAY, SEPTEMBER 22, 2019
Michigan TWO MORE CWD TSE PRION POSITIVES Total Now At 124 Positive
THURSDAY, SEPTEMBER 05, 2019
Unique Profile of The Texas CWD TSE Prion isolates, the TSE Prion CWD, Scrapie, BSE in Livestock, and CJD in Humans
SATURDAY, SEPTEMBER 28, 2019
Texas CWD TSE Prion aka Mad Deer Disease Detected Free Range Mule Deer El Paso 145 Positive To Date
Colorado Chronic Wasting Disease Response Plan December 2018
I. Executive Summary Mule deer, white-tailed deer, elk and moose are highly valued species in North America. Some of Colorado’s herds of these species are increasingly becoming infected with chronic wasting disease (CWD). As of July 2018, at least 31 of Colorado's 54 deer herds (57%), 16 of 43 elk herds (37%), and 2 of 9 moose herds (22%) are known to be infected with CWD. Four of Colorado's 5 largest deer herds and 2 of the state’s 5 largest elk herds are infected. Deer herds tend to be more heavily infected than elk and moose herds living in the same geographic area. Not only are the number of infected herds increasing, the past 15 years of disease trends generally show an increase in the proportion of infected animals within herds as well. Of most concern, greater than a 10-fold increase in CWD prevalence has been estimated in some mule deer herds since the early 2000s; CWD is now adversely affecting the performance of these herds.
snip...
IMPORTANT PUBLIC HEALTH MESSAGE
Disease in humans resulting from CWD exposure has not been reported to date. However, public health officials cannot determine there is no risk from eating meat from infected animals. Consequently, officials recommend that people avoid exposure to CWD-infected animals. Please see the Colorado Department of Public Health and Environment website ( http://www.colorado.gov/pacific/cdphe/priondiseases ) for the most current recommendations on carcass testing and other preventive measures.
To minimize exposure to CWD and other diseases of potential concern, Colorado Parks and Wildlife (CPW) and state public health officials advise hunters not to shoot, handle or consume any deer, elk or moose that is acting abnormally or appears to be sick. When fielddressing game, wear rubber gloves and minimize the use of a bone saw to cut through the brain or spinal cord (backbone). Minimize contact with brain or spinal cord tissues, eyes, spleen or lymph nodes. Always wash hands and utensils thoroughly after dressing and processing game meat.
(the map on page 71, cwd marked in red, is shocking...tss)
snip...see full report and more updated science on cwd tse prion here;
TUESDAY, MARCH 12, 2019
Colorado Parks and Wildlife is addressing Chronic Wasting Disease with its CWD Response Plan
FRIDAY, JULY 26, 2019
Chronic Wasting Disease in Cervids: Implications for Prion Transmission to Humans and Other Animal Species
MONDAY, FEBRUARY 25, 2019
MAD DOGS AND ENGLISHMEN BSE, SCRAPIE, CWD, CJD, TSE PRION A REVIEW 2019
WEDNESDAY, JULY 31, 2019
The agent of transmissible mink encephalopathy passaged in sheep is similar to BSE-L
Saturday, October 5, 2019
Variably protease‐sensitive prionopathy mimicking frontotemporal dementia
SATURDAY, OCTOBER 05, 2019
Creutzfeldt-Jakob disease (CJD) biannual update (August 2019) Health Protection Report Volume 13 Number 28 9 August 2019
ok, put you tinfoil hat on...I SAID THIS OVER 2 DECADES AGO.
-----Original Message-----
From: Terry Singeltary <flounder9@verizon.net>
To: flounder9 <flounder9@verizon.net>
Sent: Sun, May 26, 2019 10:21 am
Subject: Arguments for Alzheimer’s and Parkinson’s diseases caused by prions Stanley B. Prusiner
''From a large array of bioassays, we conclude that AD, PD, MSA, and the frontotemporal dementias, including PSP and CBD, are all prion diseases''
https://www.tandfonline.com/doi/full/10.1080/19336896.2019.1615197
From: Terry Singeltary <flounder9@verizon.net>
To: flounder9 <flounder9@verizon.net>
Sent: Sun, May 26, 2019 10:21 am
Subject: Arguments for Alzheimer’s and Parkinson’s diseases caused by prions Stanley B. Prusiner
''From a large array of bioassays, we conclude that AD, PD, MSA, and the frontotemporal dementias, including PSP and CBD, are all prion diseases''
11. Arguments for Alzheimer’s and Parkinson’s diseases caused by prions
Stanley B. Prusiner
Institute of Neurodegenerative Diseases, and Professor of Neurology and Biochemistry, University of California San Francisco
ABSTRACT
Arguments for Alzheimer’s (AD) and Parkinson’s diseases (PD) being caused by prions continue to advance with new evidence. Findings in the brains of deceased AD patients argue that both Aβ and tau prions can be demonstrated by bioassays in cultured cells as well as in transgenic (Tg) mice. Likewise, studies of the brains of deceased MSA patients have been found to contain α-synuclein prions by bioassays in cultured cells and Tg mice. Conversely, the brains of AD patients do not contain α-synuclein prions, and the brains of MSA patients do not contain Aβ or tau prions. Additionally, while the brains of patients who died of either progressive supranuclear palsy (PSP) or corticobasal degeneration (CBD) contained tau prions, neither Aβ nor α-synuclein prions were detectable. Merely measuring the levels of Aβ, tau, and α-synuclein appears to give misleading information about the etiology and pathogenesis of neurodegenerative diseases (NDs). From a large array of bioassays, we conclude that AD, PD, MSA, and the frontotemporal dementias, including PSP and CBD, are all prion diseases. Our findings argue that changes in the conformations of Aβ, tau, and α-synuclein underlie the acquisition of prion infectivity in all of these NDs.
''From a large array of bioassays, we conclude that AD, PD, MSA, and the frontotemporal dementias, including PSP and CBD, are all prion diseases''
Published: 09 September 2015
Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy
Zane Jaunmuktane, Simon Mead, Matthew Ellis, Jonathan D. F. Wadsworth, Andrew J. Nicoll, Joanna Kenny, Francesca Launchbury, Jacqueline Linehan, Angela Richard-Loendt, A. Sarah Walker, Peter Rudge, John Collinge & Sebastian Brandner
Re-Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy
>>> The only tenable public line will be that "more research is required’’ <<<
>>> possibility on a transmissible prion remains open<<<
O.K., so it’s about 23 years later, so somebody please tell me, when is "more research is required’’ enough time for evaluation ?
Re-Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy
Nature 525, 247?250 (10 September 2015) doi:10.1038/nature15369 Received 26 April 2015 Accepted 14 August 2015 Published online 09 September 2015 Updated online 11 September 2015 Erratum (October, 2015)
snip...see full Singeltary Nature comment here;
Alzheimer's disease
let's not forget the elephant in the room. curing Alzheimer's would be a great and wonderful thing, but for starters, why not start with the obvious, lets prove the cause or causes, and then start to stop that. think iatrogenic, friendly fire, or the pass it forward mode of transmission. think medical, surgical, dental, tissue, blood, related transmission. think transmissible spongiform encephalopathy aka tse prion disease aka mad cow type disease...
Commentary: Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy
Self-Propagative Replication of Ab Oligomers Suggests Potential Transmissibility in Alzheimer Disease
*** Singeltary comment PLoS ***
Alzheimer’s disease and Transmissible Spongiform Encephalopathy prion disease, Iatrogenic, what if ?
Posted by flounder on 05 Nov 2014 at 21:27 GMT
IN CONFIDENCE
5 NOVEMBER 1992
TRANSMISSION OF ALZHEIMER TYPE PLAQUES TO PRIMATES
[9. Whilst this matter is not at the moment directly concerned with the iatrogenic CJD cases from hgH, there remains a possibility of litigation here, and this presents an added complication.
There are also results to be made available shortly
(1) concerning a farmer with CJD who had BSE animals,
(2) on the possible transmissibility of Alzheimer’s and
(3) a CMO letter on prevention of iatrogenic CJD transmission in neurosurgery, all of which will serve to increase media interest.]
re-Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy
Nature 525, 247?250 (10 September 2015) doi:10.1038/nature15369 Received 26 April 2015 Accepted 14 August 2015 Published online 09 September 2015 Updated online 11 September 2015 Erratum (October, 2015)
Singeltary Comment at very bottom of this Nature publishing;
re-Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy
I would kindly like to comment on the Nature Paper, the Lancet reply, and the newspaper articles.
First, I applaud Nature, the Scientist and Authors of the Nature paper, for bringing this important finding to the attention of the public domain, and the media for printing said findings.
Secondly, it seems once again, politics is getting in the way possibly of more important Transmissible Spongiform Encephalopathy TSE Prion scientific findings. findings that could have great implications for human health, and great implications for the medical surgical arena. but apparently, the government peer review process, of the peer review science, tries to intervene again to water down said disturbing findings.
where have we all heard this before? it's been well documented via the BSE Inquiry. have they not learned a lesson from the last time?
we have seen this time and time again in England (and other Country's) with the BSE mad cow TSE Prion debacle.
That 'anonymous' Lancet editorial was disgraceful. The editor, Dick Horton is not a scientist.
The pituitary cadavers were very likely elderly and among them some were on their way to CJD or Alzheimer's. Not a bit unusual. Then the recipients ?
who got pooled extracts injected from thousands of cadavers ? were 100% certain to have been injected with both seeds. No surprise that they got both diseases going after thirty year incubations.
That the UK has a "system in place to assist science journalists" to squash embargoed science reports they find 'alarming' is pathetic.
Sounds like the journalists had it right in the first place: 'Alzheimer's may be a transmissible infection' in The Independent to 'You can catch Alzheimer's' in The Daily Mirror or 'Alzheimer's bombshell' in The Daily Express
if not for the journalist, the layperson would not know about these important findings.
where would we be today with sound science, from where we were 30 years ago, if not for the cloak of secrecy and save the industry at all cost mentality?
when you have a peer review system for science, from which a government constantly circumvents, then you have a problem with science, and humans die.
to date, as far as documented body bag count, with all TSE prion named to date, that count is still relatively low (one was too many in my case, Mom hvCJD), however that changes drastically once the TSE Prion link is made with Alzheimer's, the price of poker goes up drastically.
so, who makes that final decision, and how many more decades do we have to wait?
the iatrogenic mode of transmission of TSE prion, the many routes there from, load factor, threshold from said load factor to sub-clinical disease, to clinical disease, to death, much time is there to spread a TSE Prion to anywhere, but whom, by whom, and when, do we make that final decision to do something about it globally? how many documented body bags does it take? how many more decades do we wait? how many names can we make up for one disease, TSE prion?
Professor Collinge et al, and others, have had troubles in the past with the Government meddling in scientific findings, that might in some way involve industry, never mind human and or animal health.
FOR any government to continue to circumvent science for monetary gain, fear factor, or any reason, shame, shame on you.
in my opinion, it's one of the reasons we are at where we are at to date, with regards to the TSE Prion disease science i.e. money, industry, politics, then comes science, in that order.
greed, corporate, lobbyist there from, and government, must be removed from the peer review process of sound science, it's bad enough having them in the pharmaceutical aspect of healthcare policy making, in my opinion.
my mother died from confirmed hvCJD, and her brother (my uncle) Alzheimer's of some type (no autopsy?). just made a promise, never forget, and never let them forget, before I do.
I kindly wish to remind the public of the past, and a possible future we all hopes never happens again. ...
[9. Whilst this matter is not at the moment directly concerned with the iatrogenic CJD cases from hgH, there remains a possibility of litigation here, and this presents an added complication. There are also results to be made available shortly (1) concerning a farmer with CJD who had BSE animals, (2) on the possible transmissibility of Alzheimer's and (3) a CMO letter on prevention of iatrogenic CJD transmission in neurosurgery, all of which will serve to increase media interest.]
Singeltary Comment at very bottom of this Nature publishing;
THURSDAY, FEBRUARY 7, 2019
In Alzheimer's Mice, Decades-Old Human Cadaveric Pituitary Growth Hormone Samples Can Transmit and Seed Amyloid-Beta Pathology
Subject: CWD GSS TSE PRION SPINAL CORD, Confucius Ponders, What if?
REVIEW
***> In conclusion, sensory symptoms and loss of reflexes in Gerstmann-Sträussler-Scheinker syndrome can be explained by neuropathological changes in the spinal cord. We conclude that the sensory symptoms and loss of lower limb reflexes in Gerstmann-Sträussler-Scheinker syndrome is due to pathology in the caudal spinal cord. <***
***> The clinical and pathological presentation in macaques was mostly atypical, with a strong emphasis on spinal cord pathology.<***
***> The notion that CWD can be transmitted orally into both new-world and old-world non-human primates asks for a careful reevaluation of the zoonotic risk of CWD. <***
***> All animals have variable signs of prion neuropathology in spinal cords and brains and by supersensitive IHC, reaction was detected in spinal cord segments of all animals.<***
***> In particular the US data do not clearly exclude the possibility of human (sporadic or familial) TSE development due to consumption of venison. The Working Group thus recognizes a potential risk to consumers if a TSE would be present in European cervids.'' Scientific opinion on chronic wasting disease (II) <***
Saturday, February 2, 2019
CWD GSS TSE PRION SPINAL CORD, Confucius Ponders, What if?
Wednesday, January 16, 2019
Multiple system atrophy prions replicate in Tg(SNCAA53T) mice and induce glial pathology throughout the limbic system
TUESDAY, JANUARY 1, 2019
CHILDHOOD EXPOSURE TO CADAVERIC DURA
FRIDAY, DECEMBER 14, 2018
Transmission of amyloid-β protein pathology from cadaveric pituitary growth hormone December 14, 2018
Tuesday, December 12, 2017
Neuropathology of iatrogenic Creutzfeldt–Jakob disease and immunoassay of French cadaver-sourced growth hormone batches suggest possible transmission of tauopathy and long incubation periods for the transmission of Abeta pathology
http://tauopathies.blogspot.com/2017/12/neuropathology-of-iatrogenic.html
Neuropathology of iatrogenic Creutzfeldt–Jakob disease and immunoassay of French cadaver-sourced growth hormone batches suggest possible transmission of tauopathy and long incubation periods for the transmission of Abeta pathology
http://tauopathies.blogspot.com/2017/12/neuropathology-of-iatrogenic.html
Friday, January 29, 2016
Synucleinopathies: Past, Present and Future, iatrogenic, what if?
FRIDAY, JANUARY 10, 2014
vpspr, sgss, sffi, TSE, an iatrogenic by-product of gss, ffi, familial type prion disease, what it ???
Greetings Friends, Neighbors, and Colleagues,
vpspr, sgss, sffi, TSE, an iatrogenic by-product of gss, ffi, familial type prion disease, what it ???
Confucius is confused again.
I was just sitting and thinking about why there is no genetic link to some of these TSE prion sGSS, sFFi, and it’s really been working on my brain, and then it hit me today.
what if, vpspr, sgss, sffi, TSE prion disease, was a by-product from iatrogenic gss, ffi, familial type prion disease ???
it could explain the cases of no genetic link to the gss, ffi, familial type prion disease, to the family.
sporadic and familial is a red herring, in my opinion, and underestimation is spot on, due to the crude prehistoric diagnostic procedures and criteria and definition of a prion disease.
I say again, what if, iatrogenic, what if, with all these neurological disorders, with a common denominator that is increasingly showing up in the picture, called the prion.
I urge all scientist to come together here, with this as the utmost of importance about all these neurological disease that are increasingly showing up as a prion mechanism, to put on the front burners, the IATROGENIC aspect and the potential of transmission there from, with diseases/disease??? in question.
by definition, could they be a Transmissible Spongiform Encephalopathy TSE prion type disease, and if so, what are the iatrogenic chances of transmission?
this is very important, and should be at the forefront of research, and if proven, could be a monumental breakthrough in science and battle against the spreading of these disease/diseases.
the US National Library of Medicine National Institutes of Health pub-med site, a quick search of the word SPORADIC will give you a hit of 40,747. of those, there are a plethora of disease listed under sporadic. sporadic simply means (UNKNOWN).
the US National Library of Medicine National Institutes of Health pub-med site, a quick search of the word FAMILIAL will give you a hit of 921,815. of those, there are a plethora of disease listed under familial.
again, sporadic and familial is a red herring, in my opinion.
also, in my opinion, when you start have disease such as sporadic Fatal Familial Insomnia, (and or sporadic GSS, or the VPSPr type prion disease), and there is NO familial genetic linkage to the family of the diseased, I have serious questions there as to a familial type disease, and thus, being defined as such.
snip...see full text;
Friday, January 10, 2014
vpspr, sgss, sffi, TSE, an iatrogenic by-product of gss, ffi, familial type prion disease, what it ???
P132 Aged cattle brain displays Alzheimer’s-like pathology that can be propagated in a prionlike manner
Ines Moreno-Gonzalez (1), George Edwards III (1), Rodrigo Morales (1), Claudia Duran-Aniotz (1), Mercedes Marquez (2), Marti Pumarola (2), Claudio Soto (1)
snip...
These results may contribute to uncover a previously unsuspected etiology surrounding some cases of sporadic AD. However, the early and controversial stage of the field of prion-like transmission in non-prion diseases added to the artificial nature of the animal models utilized for these studies, indicate that extrapolation of the results to humans should not be done without further experiments.
P75 Determining transmissibility and proteome changes associated with abnormal bovine prionopathy
Dudas S (1,2), Seuberlich T (3), Czub S (1,2)
In prion diseases, it is believed that altered protein conformation encodes for different pathogenic strains. Currently 3 different strains of bovine spongiform encephalopathy (BSE) are confirmed. Diagnostic tests for BSE are able to identify animals infected with all 3 strains, however, several diagnostic laboratories have reported samples with inconclusive results which are challenging to classify. It was suggested that these may be novel strains of BSE; to determine transmissibility, brain material from index cases were inoculated into cattle.
In the first passage, cattle were intra-cranially challenged with brain homogenate from 2 Swiss animals with abnormal prionopathy. The challenged cattle incubated for 3 years and were euthanized with no clinical signs of neurologic disease. Animals were negative when tested on validated diagnostic tests but several research methods demonstrated changes in the prion conformation in these cattle, including density gradient centrifugation and immunohistochemistry. Currently, samples from the P1 animals are being tested for changes in protein levels using 2-D Fluorescence Difference Gel Electrophoresis (2D DIGE) and mass spectrometry. It is anticipated that, if a prionopathy is present, this approach should identify pathways and targets to decipher the source of altered protein conformation. In addition, a second set of cattle have been challenged with brain material from the first passage. Ideally, these cattle will be given a sufficient incubation period to provide a definitive answer to the question of transmissibility.
=====prion 2018===
***however in 1 C-type challenged animal, Prion 2015 Poster Abstracts
S67 PrPsc was not detected using rapid tests for BSE.
***Subsequent testing resulted in the detection of pathologic lesion in unusual brain location and PrPsc detection by PMCA only.
*** IBNC Tauopathy or TSE Prion disease, it appears, no one is sure ***
Posted by Terry S. Singeltary Sr. on 03 Jul 2015 at 16:53 GMT
P.9.21
Molecular characterization of BSE in Canada
Jianmin Yang 1 , Sandor Dudas 2 , Catherine Graham 2 , Markus Czub 3 , Tim McAllister 1 , Stefanie Czub 1 1 Agriculture and Agri-Food Canada Research Centre, Canada; 2 National and OIE BSE Reference Laboratory, Canada; 3 University of Calgary, Canada
Background: Three BSE types (classical and two atypical) have been identified on the basis of molecular characteristics of the misfolded protein associated with the disease. To date, each of these three types have been detected in Canadian cattle. Objectives: This study was conducted to further characterize the 16 Canadian BSE cases based on the biochemical properties of there associated PrPres.
Methods: Immuno-reactivity, molecular weight, glycoform profiles and relative proteinase K sensitivity of the PrPres from each of the 16 confirmed Canadian BSE cases was determined using modified Western blot analysis.
Results: Fourteen of the 16 Canadian BSE cases were C type, 1 was H type and 1 was L type. The Canadian H and L-type BSE cases exhibited size shifts and changes in glycosylation similar to other atypical BSE cases. PK digestion under mild and stringent conditions revealed a reduced protease resistance of the atypical cases compared to the C-type cases. N terminal-specific antibodies bound to PrPres from H type but not from C or L type. The C-terminal-specific antibodies resulted in a shift in the glycoform profile and detected a fourth band in the Canadian H-type BSE.
Discussion: The C, L and H type BSE cases in Canada exhibit molecular characteristics similar to those described for classical and atypical BSE cases from Europe and Japan. This supports the theory that the importation of BSE contaminated feedstuff is the source of C-type BSE in Canada. It also suggests a similar cause or source for atypical BSE in these countries.
Discussion: The C, L and H type BSE cases in Canada exhibit molecular characteristics similar to those described for classical and atypical BSE cases from Europe and Japan.
*** This supports the theory that the importation of BSE contaminated feedstuff is the source of C-type BSE in Canada.
*** It also suggests a similar cause or source for atypical BSE in these countries. ***
see page 176 of 201 pages...tss
*** Singeltary reply ; Molecular, Biochemical and Genetic Characteristics of BSE in Canada Singeltary reply;
On behalf of the Scientific Committee, I am pleased to inform you that your abstract
'Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009'
WAS accepted for inclusion in the INTERNATIONAL SCIENTIFIC EXCHANGE (ISE) section of the 14th International Congress on Infectious Diseases. Accordingly, your abstract will be included in the "Intl. Scientific Exchange abstract CD-rom" of the Congress which will be distributed to all participants.
Abstracts accepted for INTERNATIONAL SCIENTIFIC EXCHANGE are NOT PRESENTED in the oral OR poster sessions.
Your abstract below was accepted for: INTERNATIONAL SCIENTIFIC EXCHANGE
#0670: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Author: T. Singeltary; Bacliff, TX/US
Topic: Emerging Infectious Diseases Preferred type of presentation: International Scientific Exchange
This abstract has been ACCEPTED.
#0670: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Authors: T. Singeltary; Bacliff, TX/US
Title: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Body: Background
An update on atypical BSE and other TSE in North America. Please remember, the typical U.K. c-BSE, the atypical l-BSE (BASE), and h-BSE have all been documented in North America, along with the typical scrapie's, and atypical Nor-98 Scrapie, and to date, 2 different strains of CWD, and also TME. All these TSE in different species have been rendered and fed to food producing animals for humans and animals in North America (TSE in cats and dogs ?), and that the trading of these TSEs via animals and products via the USA and Canada has been immense over the years, decades.
Methods
12 years independent research of available data
Results
I propose that the current diagnostic criteria for human TSEs only enhances and helps the spreading of human TSE from the continued belief of the UKBSEnvCJD only theory in 2009. With all the science to date refuting it, to continue to validate this old myth, will only spread this TSE agent through a multitude of potential routes and sources i.e. consumption, medical i.e., surgical, blood, dental, endoscopy, optical, nutritional supplements, cosmetics etc.
Conclusion
I would like to submit a review of past CJD surveillance in the USA, and the urgent need to make all human TSE in the USA a reportable disease, in every state, of every age group, and to make this mandatory immediately without further delay. The ramifications of not doing so will only allow this agent to spread further in the medical, dental, surgical arena's. Restricting the reporting of CJD and or any human TSE is NOT scientific. Iatrogenic CJD knows NO age group, TSE knows no boundaries.
I propose as with Aguzzi, Asante, Collinge, Caughey, Deslys, Dormont, Gibbs, Gajdusek, Ironside, Manuelidis, Marsh, et al and many more, that the world of TSE Transmissible Spongiform Encephalopathy is far from an exact science, but there is enough proven science to date that this myth should be put to rest once and for all, and that we move forward with a new classification for human and animal TSE that would properly identify the infected species, the source species, and then the route.
Keywords: Transmissible Spongiform Encephalopathy Creutzfeldt Jakob Disease Prion
page 114 ;
http://ww2.isid.org/Downloads/14th_ICID_ISE_Abstracts.pdf
http://www.isid.org/14th_icid/
http://www.isid.org/publications/ICID_Archive.shtml
http://ww2.isid.org/Downloads/IMED2009_AbstrAuth.pdf
'Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009'
WAS accepted for inclusion in the INTERNATIONAL SCIENTIFIC EXCHANGE (ISE) section of the 14th International Congress on Infectious Diseases. Accordingly, your abstract will be included in the "Intl. Scientific Exchange abstract CD-rom" of the Congress which will be distributed to all participants.
Abstracts accepted for INTERNATIONAL SCIENTIFIC EXCHANGE are NOT PRESENTED in the oral OR poster sessions.
Your abstract below was accepted for: INTERNATIONAL SCIENTIFIC EXCHANGE
#0670: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Author: T. Singeltary; Bacliff, TX/US
Topic: Emerging Infectious Diseases Preferred type of presentation: International Scientific Exchange
This abstract has been ACCEPTED.
#0670: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Authors: T. Singeltary; Bacliff, TX/US
Title: Transmissible Spongiform encephalopathy (TSE) animal and human TSE in North America update October 2009
Body: Background
An update on atypical BSE and other TSE in North America. Please remember, the typical U.K. c-BSE, the atypical l-BSE (BASE), and h-BSE have all been documented in North America, along with the typical scrapie's, and atypical Nor-98 Scrapie, and to date, 2 different strains of CWD, and also TME. All these TSE in different species have been rendered and fed to food producing animals for humans and animals in North America (TSE in cats and dogs ?), and that the trading of these TSEs via animals and products via the USA and Canada has been immense over the years, decades.
Methods
12 years independent research of available data
Results
I propose that the current diagnostic criteria for human TSEs only enhances and helps the spreading of human TSE from the continued belief of the UKBSEnvCJD only theory in 2009. With all the science to date refuting it, to continue to validate this old myth, will only spread this TSE agent through a multitude of potential routes and sources i.e. consumption, medical i.e., surgical, blood, dental, endoscopy, optical, nutritional supplements, cosmetics etc.
Conclusion
I would like to submit a review of past CJD surveillance in the USA, and the urgent need to make all human TSE in the USA a reportable disease, in every state, of every age group, and to make this mandatory immediately without further delay. The ramifications of not doing so will only allow this agent to spread further in the medical, dental, surgical arena's. Restricting the reporting of CJD and or any human TSE is NOT scientific. Iatrogenic CJD knows NO age group, TSE knows no boundaries.
I propose as with Aguzzi, Asante, Collinge, Caughey, Deslys, Dormont, Gibbs, Gajdusek, Ironside, Manuelidis, Marsh, et al and many more, that the world of TSE Transmissible Spongiform Encephalopathy is far from an exact science, but there is enough proven science to date that this myth should be put to rest once and for all, and that we move forward with a new classification for human and animal TSE that would properly identify the infected species, the source species, and then the route.
Keywords: Transmissible Spongiform Encephalopathy Creutzfeldt Jakob Disease Prion
page 114 ;
http://ww2.isid.org/Downloads/14th_ICID_ISE_Abstracts.pdf
http://www.isid.org/14th_icid/
http://www.isid.org/publications/ICID_Archive.shtml
http://ww2.isid.org/Downloads/IMED2009_AbstrAuth.pdf
THURSDAY, AUGUST 17, 2017
*** Monitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United States revisited 2017
Singeltary et al
http://creutzfeldt-jakob-disease.blogspot.com/2017/08/monitoring-occurrence-of-emerging-forms.html
*** Monitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United States revisited 2017
Singeltary et al
http://creutzfeldt-jakob-disease.blogspot.com/2017/08/monitoring-occurrence-of-emerging-forms.html
Tuesday, March 20, 2018
Variably protease-sensitive prionopathy (VPSPr), sporadic creutzfeldt jakob disease sCJD, the same disease, what if?
UNDAY, MARCH 10, 2019
National Prion Disease Pathology Surveillance Center Cases Examined¹ Updated Feb 1, 2019 Variably protease-sensitive prionopathy VPSPr
THURSDAY, MARCH 14, 2019
USDA APHIS CDC Cervids: Chronic Wasting Disease Specifics Updated 2019
SATURDAY, MARCH 16, 2019
Chronic Wasting Disease CWD TSE Prion United States of America Update March 16, 2019
FRIDAY, MARCH 15, 2019
Saskatchewan Chronic Wasting Disease TSE Prion 349 Cases Positive for 2018
TUESDAY, MARCH 26, 2019
USDA ARS 2018 USAHA RESOLUTIONS Investigation of the Role of the Prion Protein Gene in CWD Resistance and Transmission of Disease
FRIDAY, MARCH 29, 2019
First Detection of Chronic Wasting Disease in a Wild Red Deer (Cervus elaphus) in Europe
FRIDAY, MAY 24, 2019
Assessing chronic wasting disease strain differences in free-ranging cervids across the United States
Thursday, May 23, 2019
Prion 2019 Emerging Concepts CWD, BSE, SCRAPIE, CJD, SCIENTIFIC PROGRAM Schedule and Abstracts
MONDAY, MAY 20, 2019
Tracking and clarifying differential traits of classical- and atypical L-type bovine spongiform encephalopathy prions after transmission from cattle to cynomolgus monkeys
SUNDAY, APRIL 14, 2019
Estimation of prion infectivity in tissues of cattle infected with atypical BSE by real time-quaking induced conversion assay
WEDNESDAY, APRIL 24, 2019
USDA Announces Atypical Bovine Spongiform Encephalopathy Detection Aug 29, 2018 A Review of Science 2019
Diagnosis and Reporting of Creutzfeldt-Jakob DiseaseSingeltary, Sr et al. JAMA.2001; 285: 733-734. Vol. 285 No. 6, February 14, 2001 JAMA Diagnosis and Reporting of Creutzfeldt-Jakob DiseaseTo the Editor:In their Research Letter, Dr Gibbons and colleagues1 reported that the annual US death rate due to Creutzfeldt-Jakob disease (CJD) has been stable since 1985. These estimates, however, are based only on reported cases, and do not include misdiagnosed or preclinical cases. It seems to me that misdiagnosis alone would drastically change these figures. An unknown number of persons with a diagnosis of Alzheimer disease in fact may have CJD, although only a small number of these patients receive the postmortem examination necessary to make this diagnosis. Furthermore, only a few states have made CJD reportable. Human and animal transmissible spongiform encephalopathies should be reportable nationwide and internationally..Terry S. Singeltary, Sr Bacliff, Tex1. Gibbons RV, Holman RC, Belay ED, Schonberger LB. Creutzfeldt-Jakob disease in the United States: 1979-1998. JAMA. 2000;284:2322-2323.doi:10.1016/S1473-3099(03)00715-1 Copyright © 2003 Published by Elsevier Ltd. Newsdesk
Tracking spongiform encephalopathies in North AmericaXavier BoschAvailable online 29 July 2003.Volume 3, Issue 8, August 2003, Page 463“My name is Terry S Singeltary Sr, and I live in Bacliff, Texas. I lost my mom to hvCJD (Heidenhain variant CJD) and have been searching for answers ever since. What I have found is that we have not been told the truth. CWD in deer and elk is a small portion of a much bigger problem..” ............................January 28, 2003; 60 (2) VIEWS & REVIEWSMonitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United StatesErmias D. Belay, Ryan A. Maddox, Pierluigi Gambetti, Lawrence B. SchonbergerFirst published January 28, 2003, DOI: https://doi.org/10.1212/01.WNL.0000036913.87823.D6AbstractTransmissible spongiform encephalopathies (TSEs) attracted increased attention in the mid-1980s because of the emergence among UK cattle of bovine spongiform encephalopathy (BSE), which has been shown to be transmitted to humans, causing a variant form of Creutzfeldt-Jakob disease (vCJD). The BSE outbreak has been reported in 19 European countries, Israel, and Japan, and human cases have so far been identified in four European countries, and more recently in a Canadian resident and a US resident who each lived in Britain during the BSE outbreak. To monitor the occurrence of emerging forms of CJD, such as vCJD, in the United States, the Centers for Disease Control and Prevention has been conducting surveillance for human TSEs through several mechanisms, including the establishment of the National Prion Disease Pathology Surveillance Center. Physicians are encouraged to maintain a high index of suspicion for vCJD and use the free services of the pathology center to assess the neuropathology of clinically diagnosed and suspected cases of CJD or other TSEs.Received May 7, 2002. Accepted August 28, 2002.RE-Monitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United StatesTerry S. Singeltary, retired (medically)Published March 26, 200326 March 2003Terry S. Singeltary, retired (medically) CJD WATCHI lost my mother to hvCJD (Heidenhain Variant CJD). I would like to comment on the CDC's attempts to monitor the occurrence of emerging forms of CJD. Asante, Collinge et al [1] have reported that BSE transmission to the 129-methionine genotype can lead to an alternate phenotype that is indistinguishable from type 2 PrPSc, the commonest sporadic CJD. However, CJD and all human TSEs are not reportable nationally. CJD and all human TSEs must be made reportable in every state and internationally. I hope that the CDC does not continue to expect us to still believe that the 85%+ of all CJD cases which are sporadic are all spontaneous, without route/source. We have many TSEs in the USA in both animal and man. CWD in deer/elk is spreading rapidly and CWD does transmit to mink, ferret, cattle, and squirrel monkey by intracerebral inoculation. With the known incubation periods in other TSEs, oral transmission studies of CWD may take much longer. Every victim/family of CJD/TSEs should be asked about route and source of this agent. To prolong this will only spread the agent and needlessly expose others. In light of the findings of Asante and Collinge et al, there should be drastic measures to safeguard the medical and surgical arena from sporadic CJDs and all human TSEs. I only ponder how many sporadic CJDs in the USA are type 2 PrPSc?Reply to Singletary Ryan A. Maddox, MPH Other Contributors: Published March 26, 2003Mr. Singletary raises several issues related to current Creutzfeldt- Jakob disease (CJD) surveillance activities. Although CJD is not a notifiable disease in most states, its unique characteristics, particularly its invariably fatal outcome within usually a year of onset, make routine mortality surveillance a useful surrogate for ongoing CJD surveillance.[1] In addition, because CJD is least accurately diagnosed early in the course of illness, notifiable-disease surveillance could be less accurate than, if not duplicative of, current mortality surveillance.[1] However, in states where making CJD officially notifiable would meaningfully facilitate the collection of data to monitor for variant CJD (vCJD) or other emerging prion diseases, CDC encourages the designation of CJD as a notifiable disease.[1] Moreover, CDC encourages physicians to report any diagnosed or suspected CJD cases that may be of special public health importance (e.g...., vCJD, iatrogenic CJD, unusual CJD clusters).As noted in our article, strong evidence is lacking for a causal link between chronic wasting disease (CWD) of deer and elk and human disease,[2] but only limited data seeking such evidence exist. Overall, the previously published case-control studies that have evaluated environmental sources of infection for sporadic CJD have not consistently identified strong evidence for a common risk factor.[3] However, the power of a case-control study to detect a rare cause of CJD is limited, particularly given the relatively small number of subjects generally involved and its long incubation period, which may last for decades. Because only a very small proportion of the US population has been exposed to CWD, a targeted surveillance and investigation of unusual cases or case clusters of prion diseases among persons at increased risk of exposure to CWD is a more efficient approach to detecting the possible transmission of CWD to humans. In collaboration with appropriate local and state health departments and the National Prion Disease Pathology Surveillance Center, CDC is facilitating or conducting such surveillance and case- investigations, including related laboratory studies to characterize CJD and CWD prions.Mr. Singletary also expresses concern over a recent publication by Asante and colleagues indicating the possibility that some sporadic CJD cases may be attributable to bovine spongiform encephalopathy (BSE).[4] The authors reported that transgenic mice expressing human prion protein homozygous for methionine at codon 129, when inoculated with BSE prions, developed a molecular phenotype consistent with a subtype of sporadic CJD. Although the authors implied that BSE might cause a sporadic CJD-like illness among persons homozygous for methionine, the results of their research with mice do not necessarily directly apply to the transmission of BSE to humans. If BSE causes a sporadic CJD-like illness in humans, an increase in sporadic CJD cases would be expected to first occur in the United Kingdom, where the vast majority of vCJD cases have been reported. In the United Kingdom during 1997 through 2002, however, the overall average annual mortality rate for sporadic CJD was not elevated; it was about 1 case per million population per year. In addition, during this most recent 6-year period following the first published description of vCJD in 1996, there was no increasing trend in the reported annual number of UK sporadic CJD deaths.[3, 5] Furthermore, surveillance in the UK has shown no increase in the proportion of sporadic CJD cases that are homozygous for methionine (Will RG, National CJD Surveillance Unit, United Kingdom, 2003; personal communication)..References1. Gibbons RV, Holman RC, Belay ED, Schonberger LB. Diagnosis and reporting of Creutzfeldt-Jakob disease. JAMA 2001;285:733-734.2. Belay ED, Maddox RA, Gambetti P, Schonberger LB. Monitoring the occurrence of emerging forms of Creutzfeldt-Jakob disease in the United States. Neurology 2003;60:176-181.3. Belay ED. Transmissible spongiform encephalopathies in humans. Annu Rev Microbiol 1999;53:283-314.4. Asante EA, Linehan JM, Desbruslais M, et al. BSE prions propagate as either variant CJD-like or sporadic CJD-like prion strains in transgenic mice expressing human prion protein. EMBO J 2002;21:6358-6366.5. The UK Creutzfeldt-Jakob Disease Surveillance Unit. CJD statistics. Available at: http://www.cjd.ed.ac.uk/figures.htm. Accessed February 18, 2003.Competing Interests: None declared.Volume 2: Science4. The link between BSE and vCJDSummary 4.29 The evidence discussed above that vCJD is caused by BSE seems overwhelming. Uncertainties exist about the cause of CJD in farmers, their wives and in several abattoir workers. It seems that farmers at least might be at higher risk than others in the general population. 1 Increased ascertainment (ie, increased identification of cases as a result of greater awareness of the condition) seems unlikely, as other groups exposed to risk, such as butchers and veterinarians, do not appear to have been affected. The CJD in farmers seems to be similar to other sporadic CJD in age of onset, in respect to glycosylation patterns, and in strain-typing in experimental mice. Some farmers are heterozygous for the methionine/valine variant at codon 129, and their lymphoreticular system (LRS) does not contain the high levels of PrPSc found in vCJD.***>It remains a remote possibility that when older people contract CJD from BSE the resulting phenotype is like sporadic CJD and is distinct from the vCJD phenotype in younger people...endBSE INQUIRYSATURDAY, JUNE 23, 2018CDC***> Diagnosis of Methionine/Valine Variant Creutzfeldt-Jakob Disease by Protein Misfolding Cyclic AmplificationVolume 24, Number 7—July 2018 Dispatch
Diagnosis and Reporting of Creutzfeldt-Jakob Disease
2 January 2000 British Medical Journal U.S.
Scientist should be concerned with a CJD epidemic in the U.S., as well
15 November 1999 British Medical Journal hvCJD in the USA * BSE in U.S.
MONDAY, FEBRUARY 25, 2019
MAD DOGS AND ENGLISHMEN BSE, SCRAPIE, CWD, CJD, TSE PRION A REVIEW 2019
BSE INQUIRY EVIDENCE
Why did the appearance of new TSEs in animals matter so much? It has always been known that TSEs will transfer across species boundaries. The reason for this was never known until the genetic nature of the prion gene was fully investigated and found to be involved. The gene is found to have well preserved sites and as such there is a similar gene throughout the animal kingdom...and indeed a similar gene is found in insects! It is NOT clear that the precise close nature of the PrP gene structure is essention for low species barriers. Indeed it is probably easier to infect cats with BSE than it is to infect sheep. As such it is not clear that simply because it is possible to infect BSE from cattle into certain monkeys then other apes will necessarily be infectable with the disease. One factor has stood out, however, and that is that BSE, when inoculated into mice would retain its apparent nature of disease strain, and hence when it was inoculated back into cattle, then the same disease was produced. Similarly if the TSE from kudu was inoculated into mice then a similar distribution of disease in the brain of the mouse is seen as if BSE had been inoculated into the mouse. This phenomenon was not true with scrapie, in which the transmission across a species barrier was known to lose many of the scrapie strain phenomena in terms of incubation period or disease histopathology. This also suggested that BSE was not derived from scrapie originally but we probably will never know.
------------------------------------------------------------------------
TSE in wild UK deer? The first case of BSE (as we now realise) was in a nyala in London zoo and the further zoo cases in ungulates were simply thought of as being interesting transmissions of scrapie initially. The big problem started to appear with animals in 1993-5 when it became clear that there was an increase in the CJD cases in people that had eaten deer although the statistics involved must have been questionable. The reason for this was that the CJD Surveillance was well funded to look into the diet of people dying of CJD. This effect is not clear with vCJD...if only because the numbers involved are much smaller and hence it is difficult to gain enough statistics. They found that many other foods did not appear to have much association at all but that deer certainly did and as years went by the association actually became clearer. The appearance of vCJD in 1996 made all this much more difficult in that it was suddenly clearer that the cases of sporadic CJD that they had been checking up until then probably had nothing to do with beef...and the study decreased. During the period there was an increasing worry that deer were involved with CJD..
see references:
DEER BRAIN SURVEY
Subject: Re: DEER SPONGIFORM ENCEPHALOPATHY SURVEY & HOUND STUDY
Date: Fri, 18 Oct 2002 23:12:22 +0100
From: Steve Dealler
Reply-To: Bovine Spongiform Encephalopathy Organization: Netscape Online member
To: BSE-L@ References: <3daf5023 .4080804="" a="" class="yiv7832104488linkified" fg_scanned="1" href="http://wt.net/" rel="noopener noreferrer" shape="rect" style="color: blue; cursor: pointer;" target="_blank">WT.NET
Dear Terry,
An excellent piece of review as this literature is desparately difficult to get back from Government sites.
What happened with the deer was that an association between deer meat eating and sporadic CJD was found in about 1993. The evidence was not great but did not disappear after several years of asking CJD cases what they had eaten. I think that the work into deer disease largely stopped because it was not helpful to the UK industry...and no specific cases were reported. Well, if you dont look adequately like they are in USA currenly then you wont find any!
Steve Dealler ===============
BSE Inquiry Steve Dealler
Management In Confidence
BSE: Private Submission of Bovine Brain Dealler
reports of sheep and calf carcasses dumped...
re-scrapie to cattle GAH Wells BSE Inquiry
https://web.archive.org/web/20090506043931/http://www.bseinquiry.gov.uk/files/yb/1993/12/09001001.pdf
Dr. Dealler goes rogue to confirm BSE
Confirmation BSE Dealler's mad cow
BSE vertical transmission
1993 cjd report finds relationship with eat venison and cjd increases 9 fold, let the cover up begin...tss
FINDINGS
*** The association between venison eating and risk of CJD shows similar pattern, with regular venison eating associated with a 9 FOLD INCREASE IN RISK OF CJD (p = 0.04). ***
*** The association between venison eating and risk of CJD shows similar pattern, with regular venison eating associated with a 9 FOLD INCREASE IN RISK OF CJD (p = 0.04). ***
*** The association between venison eating and risk of CJD shows similar pattern, with regular venison eating associated with a 9 FOLD INCREASE IN RISK OF CJD (p = 0.04). ***
There is some evidence that risk of CJD INCREASES WITH INCREASING FREQUENCY OF LAMB EATING (p = 0.02)..
The evidence for such an association between beef eating and CJD is weaker (p = 0.14). When only controls for whom a relative was interviewed are included, this evidence becomes a little STRONGER (p = 0.08).
snip...
It was found that when veal was included in the model with another exposure, the association between veal and CJD remained statistically significant (p = < 0.05 for all exposures), while the other exposures ceased to be statistically significant (p = > 0.05).
snip...
In conclusion, an analysis of dietary histories revealed statistical associations between various meats/animal products and INCREASED RISK OF CJD. When some account was taken of possible confounding, the association between VEAL EATING AND RISK OF CJD EMERGED AS THE STRONGEST OF THESE ASSOCIATIONS STATISTICALLY. ...
snip...
In the study in the USA, a range of foodstuffs were associated with an increased risk of CJD, including liver consumption which was associated with an apparent SIX-FOLD INCREASE IN THE RISK OF CJD. By comparing the data from 3 studies in relation to this particular dietary factor, the risk of liver consumption became non-significant with an odds ratio of 1.2 (PERSONAL COMMUNICATION, PROFESSOR A. HOFMAN. ERASMUS UNIVERSITY, ROTTERDAM). (???...TSS)
snip...see full report ;
GAME FARM INDUSTRY WANTS TO COVER UP FINDINGS OF INCREASE RISK TO CJD FROM CERVID
BSE INQUIRY
CJD9/10022
October 1994
Mr R.N. Elmhirst Chairman British Deer Farmers Association Holly Lodge Spencers Lane
BerksWell Coventry CV7 7BZ
Dear Mr Elmhirst,
CREUTZFELDT-JAKOB DISEASE (CJD) SURVEILLANCE UNIT REPORT
Thank you for your recent letter concerning the publication of the third annual report from the CJD Surveillance Unit. I am sorry that you are dissatisfied with the way in which this report was published.
The Surveillance Unit is a completely independant outside body and the Department of Health is committed to publishing their reports as soon as they become available. In the circumstances it is not the practice to circulate the report for comment since the findings of the report would not be amended.. In future we can ensure that the British Deer Farmers Association receives a copy of the report in advance of publication.
The Chief Medical Officer has undertaken to keep the public fully informed of the results of any research in respect of CJD. This report was entirely the work of the unit and was produced completely independantly of the the Department.
The statistical results reqarding the consumption of venison was put into perspective in the body of the report and was not mentioned at all in the press release. Media attention regarding this report was low key but gave a realistic presentation of the statistical findings of the Unit. This approach to publication was successful in that consumption of venison was highlighted only once by the media ie. in the News at one television proqramme.
I believe that a further statement about the report, or indeed statistical links between CJD and consumption of venison, would increase, and quite possibly give damaging credence, to the whole issue. From the low key media reports of which I am aware it seems unlikely that venison consumption will suffer adversely, if at all.
snip...see full text;
MONDAY, FEBRUARY 25, 2019
MAD DOGS AND ENGLISHMEN BSE, SCRAPIE, CWD, CJD, TSE PRION A REVIEW 2019
SATURDAY, MARCH 2, 2019
MAD COW TSE PRION DISEASE AND THE PEER REVIEW PROCESS OF BSe Science $$$
friendly fire, pass it forward, they call it iatrogenic cjd, or what i call 'tse prion poker', are you all in $$$
SATURDAY, MARCH 16, 2019
Medical Devices Containing Materials Derived from Animal Sources (Except for In Vitro Diagnostic Devices) Guidance for Industry and Food and Drug Administration Staff Document issued on March 15, 2019 Singeltary Submission
TUESDAY, APRIL 09, 2019
Horizon Health Network Moncton Hospital notified more than 700 patients after two cases of CJD were diagnosed both patients had undergone cataracts surgery before being diagnosed
MONDAY, APRIL 8, 2019
Studies Further Support Transmissibility of Alzheimer Disease–Associated Proteins
SUNDAY, MAY 26, 2019
Arguments for Alzheimer’s and Parkinson’s diseases caused by prions Stanley B. Prusiner
''From a large array of bioassays, we conclude that AD, PD, MSA, and the frontotemporal dementias, including PSP and CBD, are all prion diseases''
WASTED DAYS AND WASTED NIGHTS...FREDDY FENDER
Terry S. Singeltary Sr.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.